|
Back to 2011 Program
The Use of Magnetic Resonance Angiography for Vascularized Groin Lymph Node Transfer: An Anatomic Study
Erez Dayan, M.D., Mark Smith, M.D., Alex Kagen, M.D., Joseph H. Dayan, M.D..
Beth Israel Medical Center, New York, NY, USA.
Background
Postmastectomy lymphedema is a challenging problem with a reported incidence of 20% following axillary node dissection. Vascularized groin lymph node transfer has been successfully used to treat lymphedema. This involves transfer of the superficial inguinal lymph nodes supplied by the superficial circumflexiliac artery. However, there is sparse literature on the anatomic basis of thisflap and no reported literature on Magnetic Resonance Angiography (MRA) for preoperative planning. The purpose of this study was to clarify the anatomy using MRA in order to provide practical guidelines for capturing the superficial inguinal nodes when designing this flap.
Methods
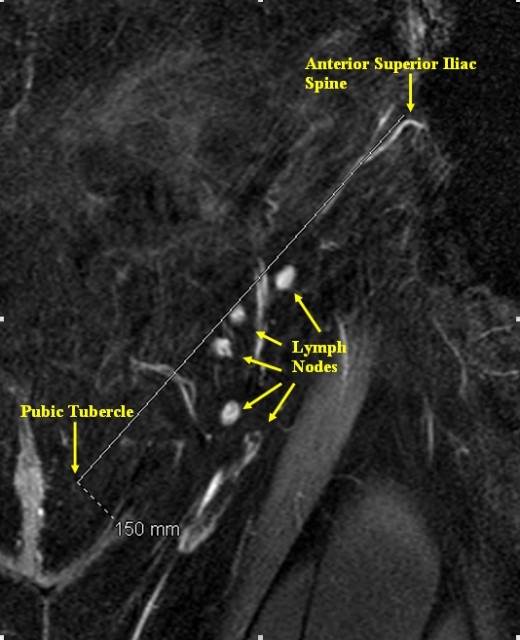
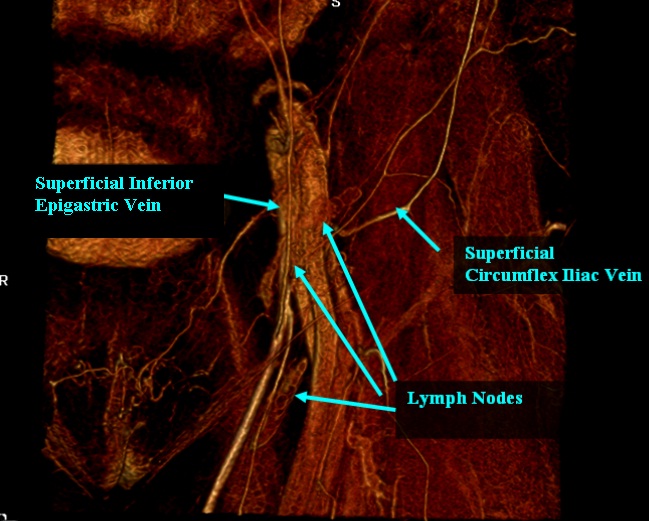
MRA was used on 87 patients to identify the bilateral superficial inguinal lymph nodes. Using coronal sections, a line was marked from the anterior superior iliac spine (ASIS) to the pubic tubercle, corresponding to the inguinal ligament. The coordinates of each lymph node were plotted along this ‘x’ axis and along a line perpendicular to this ‘x’ axis. The relationship of the nodes to the superficial inferior epigastric vein (SIEV) and superficial circumflex iliac vein (SCIV) was also evaluated.
Results
1,449 distinct superficial inguinal groin lymph nodes were identified. There was an average of 8.3 superficial nodes per groin clustered into a horizontal and vertical chain. The mean distance of the nodes from the ASIS toward the pubic tubercle was 9.2 cm (SD = 2.7) and 3.0 cm (SD = 1.9) below the inguinal ligament. This correlates to one-third the distance along the inguinal ligamentfrom the pubic tubercle. 68% of the lymph nodes were located within a 3 cm radius of this epicenter. The superficial nodes tended to cluster at the junction of the SIEV and the SCIV: 67% within this venous bifurcation, 14% just inferior to the SCIV, and 19% medial to the SIEV.
Conclusions
The results in this study provide a practical guide to capturing the superficial inguinal nodes by using readily identifiable landmarks such as the ASIS, pubictubercle, SIEV, and SCIV. Preoperative MRA may also provide the surgeon within sight as to which is the ideal side for node harvest and ensure adequate nodal tissue is captured in the flap. 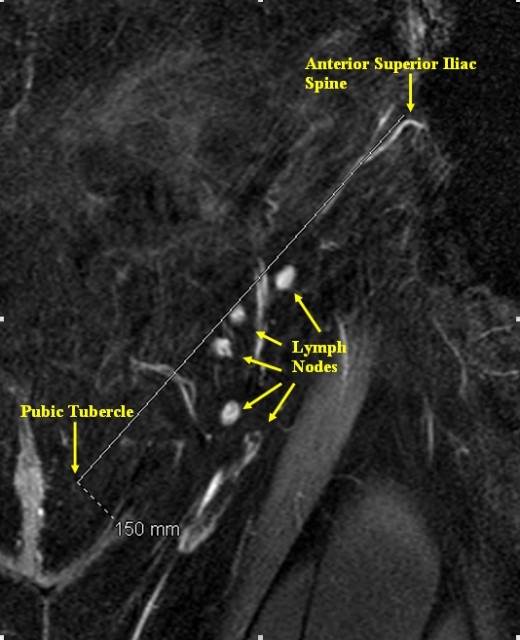 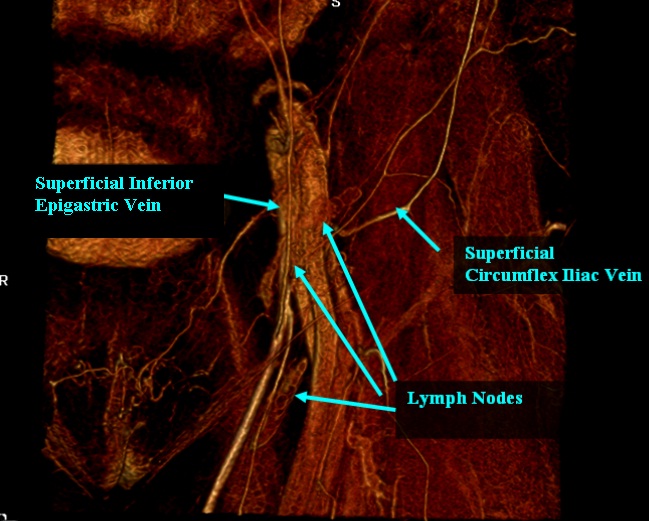
Back to 2011 Program
|