|
|
 |
Back to 2011 Program
Systematic review of patient-reported outcomes measures to assess quality of life in cleft lip and palate patients
Donna A. Eckstein, BA, Rebecca L. Wu, BS, Takintope Akinbiyi, BS, MSc, Lester Silver, MD, Peter J. Taub, MD.
Mount Sinai School of Medicine, New York, NY, USA.
Background:
Patient-reported outcomes in the treatment of cleft lip and palate (CLP) are a critical aspect of clinical research. Traditional surgical outcomes evaluations for CLP patients have focused on objective measures such as photographs, facial measurements and morbidity and mortality. Although these measures remain important, they leave many questions unanswered. Instead, patient-reported outcomes measures (PROMs) that include aesthetic results, speech, functionality, self-image, incorporation into society, and quality of life provide a more thorough assessment of surgical outcomes. Therefore, it is vital that reliable and valid questionnaires are available to surgeons caring for CLP patients. In this review we assess the currently available CLP PROMs in terms of validity and reliability, as well as domains analyzed by these instruments.
Methods:
The authors performed a systematic literature review to identify PROMs validated for use in CLP patients. The databases, Medline, CINAHL, and PsychINFO were searched using the terms: cleft, cleft surgery, quality of life, patient satisfaction, and questionnaire. All instruments included were identified as PROMs assessing quality of life and/or patient satisfaction in CLP patients. Qualifying instruments were assessed for adherence to international guidelines for health outcomes instrument development and validation set by the Scientific Advisory Committee of the Medical Outcomes Trust as well as for the scope of their content.
Results:
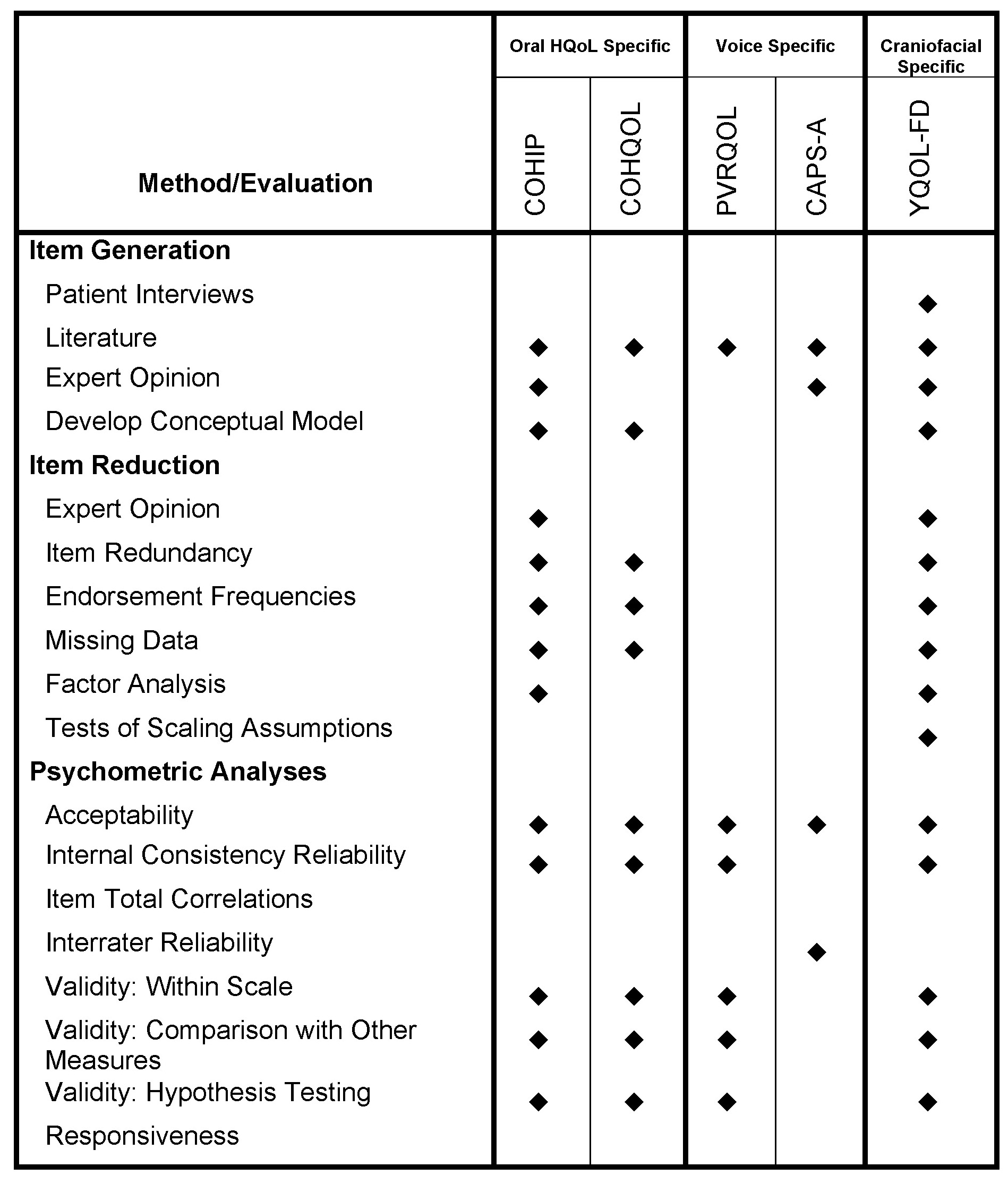
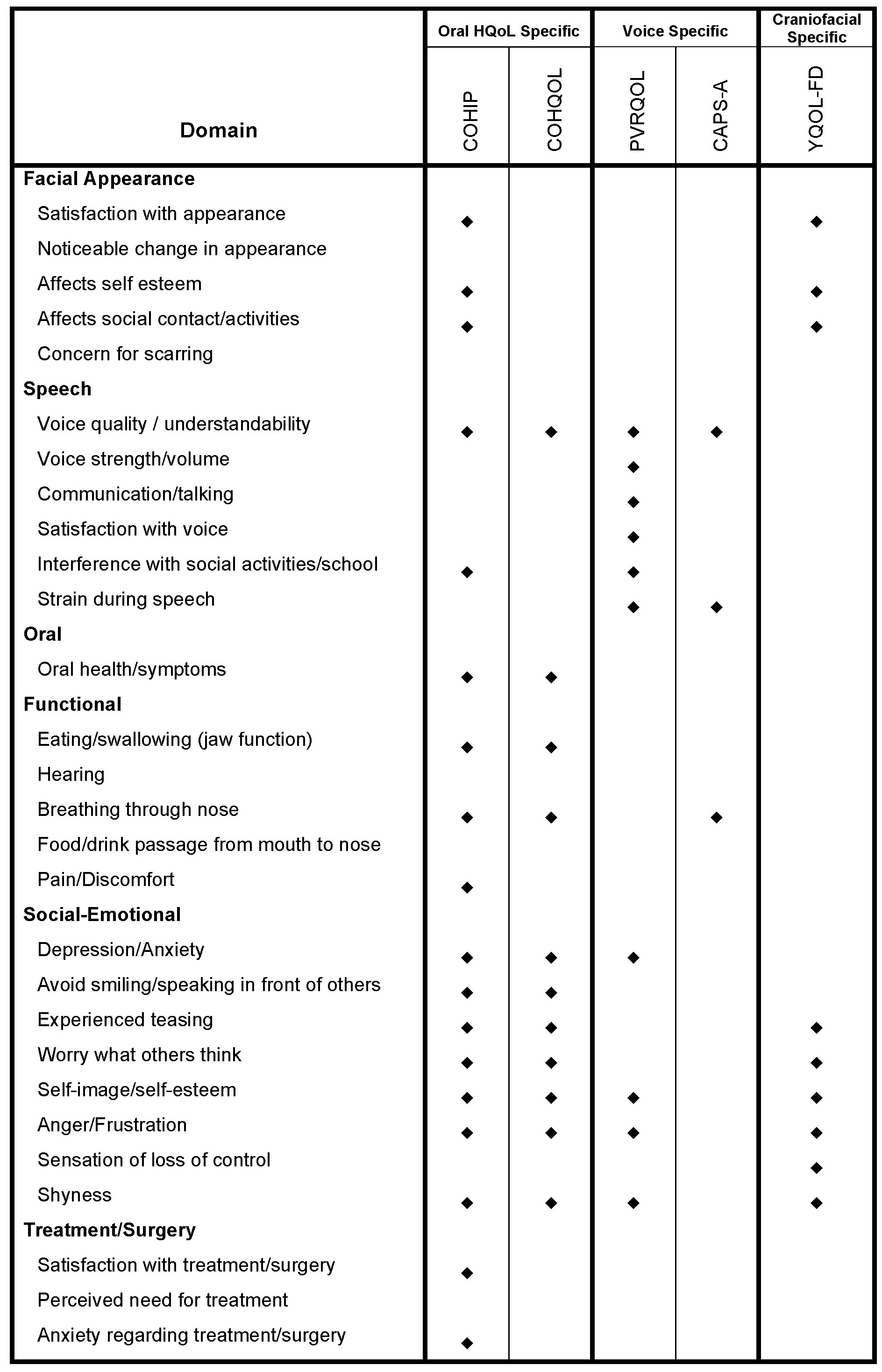
The authors identified 44 PROMs used in CLP studies. After 15 ad hoc questionnaires, eight generic instruments, 11 psychiatric instruments, and one non-English language questionnaire were excluded nine measures remained. Of these, four were never validated in the cleft population. Analysis of the remaining five measures revealed that there is one craniofacial specific measure, the Youth Quality of Life - Facial Differences (YQOL-FD), two voice-related measures, the Patient Voice-Related Quality of Life Survey (PVRQOL) and Cleft Audit Protocol for Speech - Augmented (CAPS-A), and two oral health-related measures, the Child Oral Health Impact Profile (COHIP) and Child Oral Health Quality of Life Questionnaire (COHQOL), that were validated in the cleft population. Of these, the YQOL-FD, COHIP, and COHQOL were sufficiently validated according to guidelines (Table 1). None of the questionnaires were tested for responsiveness, the ability to detect change over time, which is an important aspect of outcomes research, particularly for patients currently undergoing treatment. Of these questionnaires, none were created with the cleft population specifically in mind, resulting in significant content limitations (Table 2). Specifically, information regarding surgical experience and satisfaction and cleft palate-related functional issues are missing.
Conclusions:
This review highlights the lack of comprehensive, valid, reliable, and responsive instruments with which to measure patient-reported outcomes in CLP surgery. To allow for thorough assessment of satisfaction and quality of life in these patients following surgery, further research to methodically develop and validate new CLP surgery-specific instruments is needed. 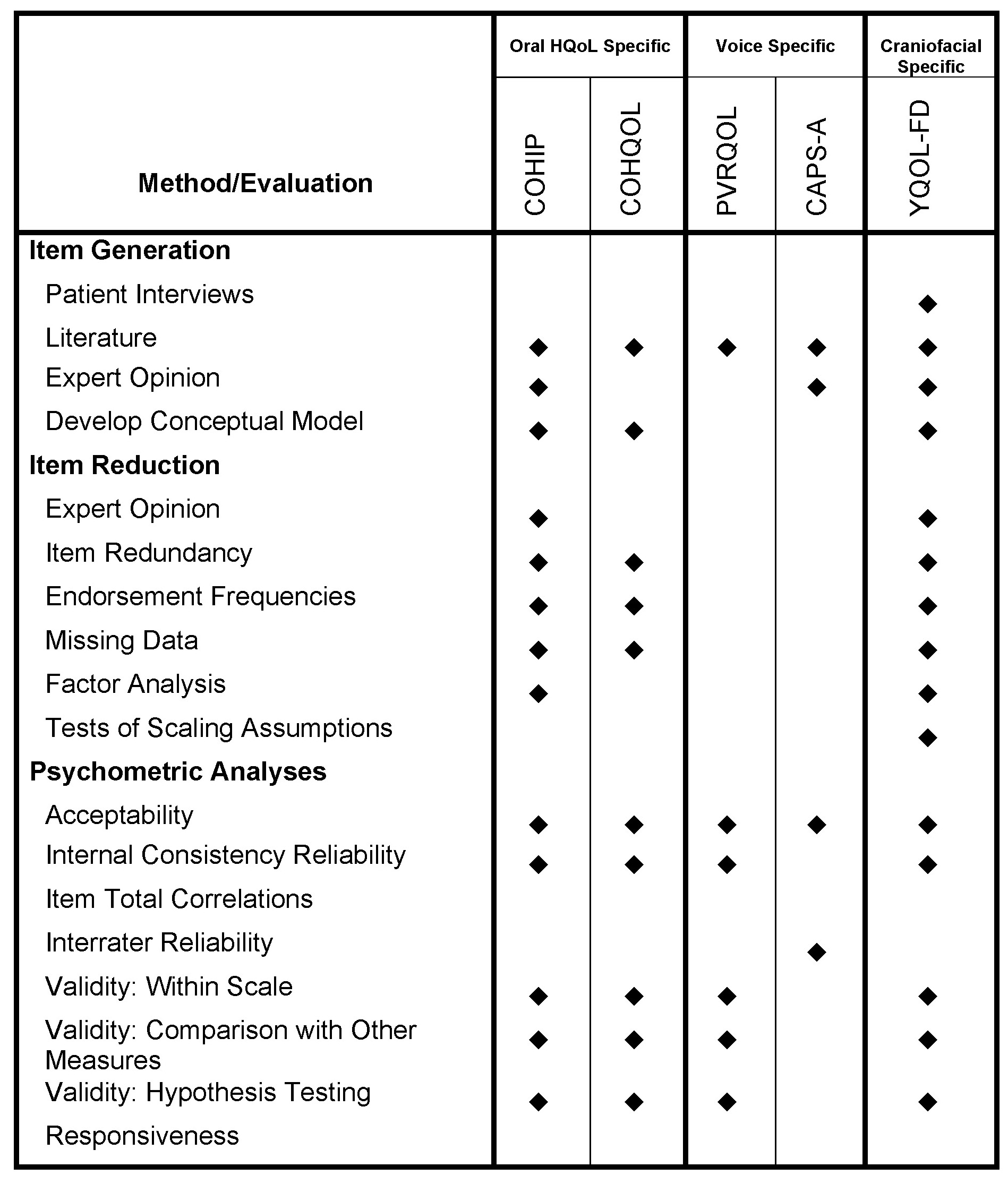 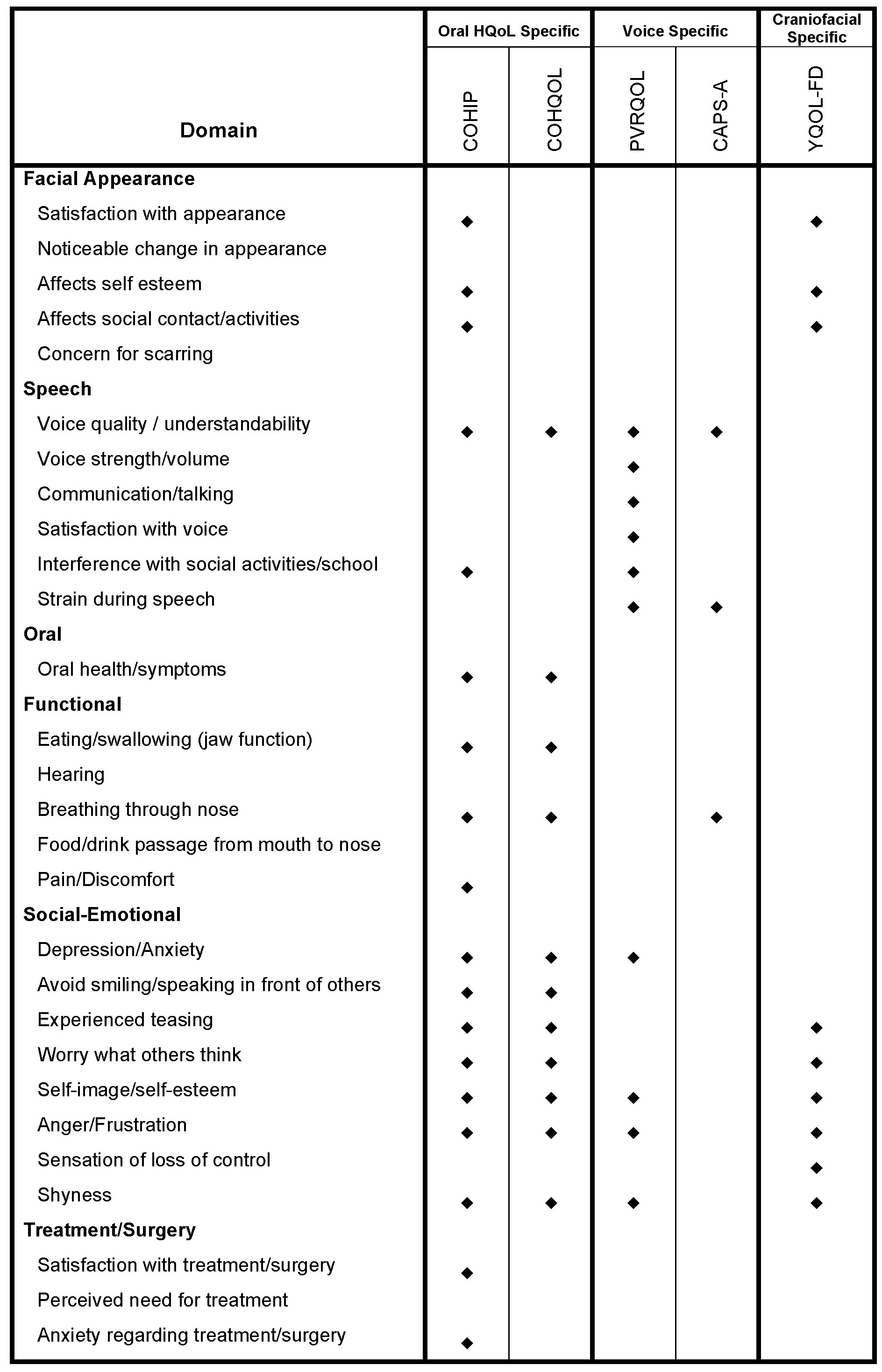
Back to 2011 Program
|