|
|
 |
Back to 2011 Program
Optimizing Flap Choice in the Complex Groin Wound: A Review of 175 Consecutive Cases
Michael N. Mirzabeigi, MS, Shareef Jandali, MD, John Fischer, MD, Jennifer McGrath, MD, Stephen J. Kovach, MD, Liza C. Wu, MD, David W. Low, MD, Joseph M. Serletti, MD, Suhail Kanchwala, MD.
University of Pennsylvania, Philadelphia, PA, USA.
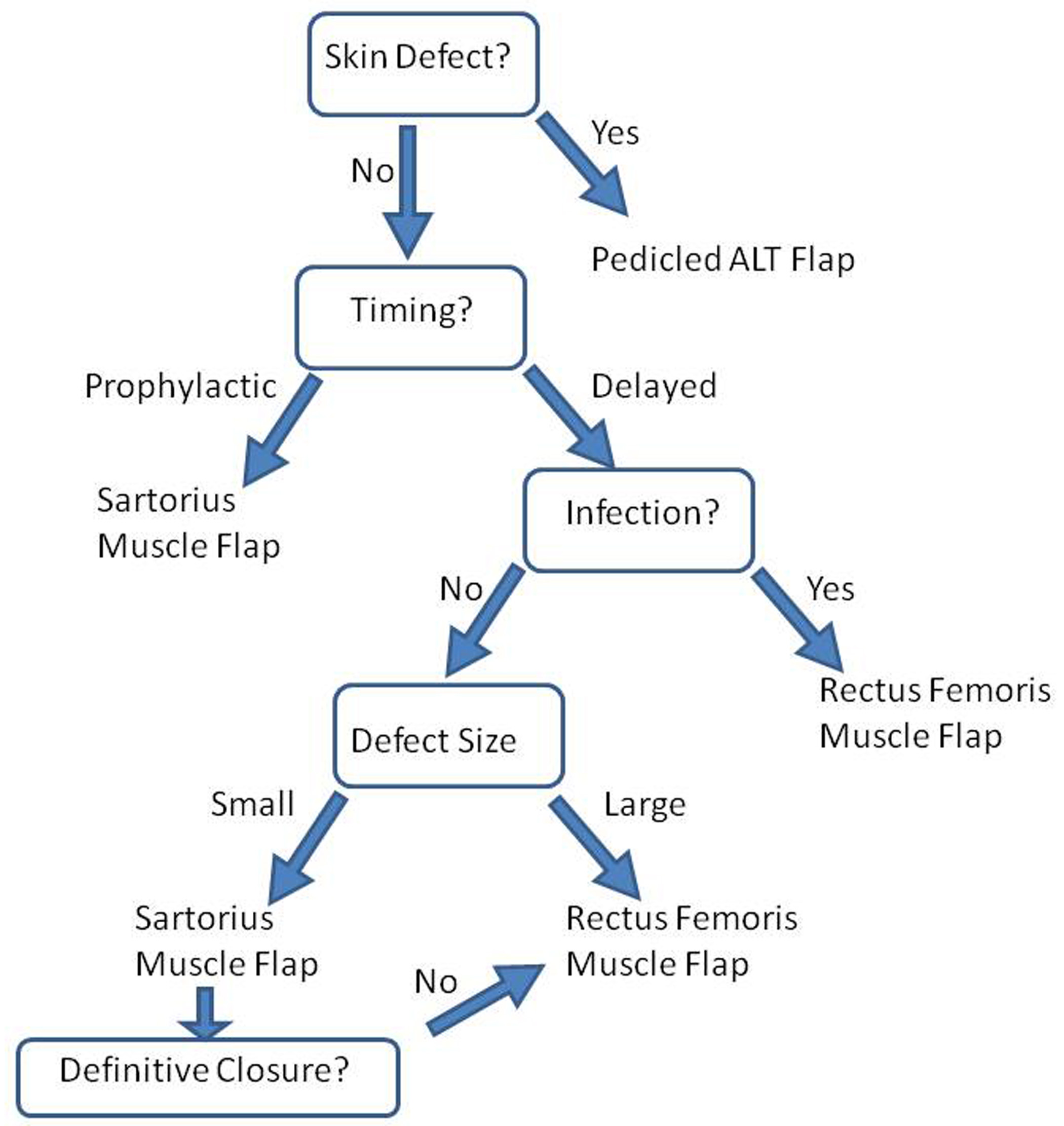
BACKGROUND: Complex groin wounds following vascular surgery can be both life- and limb-threatening. Aggressive debridement in conjunction with muscle flap coverage stands as an effective approach when managing these wounds. The sartorius (SMF), rectus femoris (RF), gracilis, and ALT/vastus lateralis flaps have all been utilized for wound coverage at our institution, with the RF and SMF serving as workhorse flaps. The purpose of this study is to assess the clinical outcomes of a large cohort of patients with complex groin wounds and describe an evidence-based algorithm for flap selection.
METHODS: A retrospective review of records was performed on patients undergoing reconstruction for a complex groin wound from January 2005 to December 2010. The outcomes assessment was subdivided by wound etiology with a focus on comparing the RF and SMF.
RESULTS: 175 consecutive flaps for complex groin wound coverage were identified following a consultation request by the vascular surgery service. Flap selection was based on the timing of reconstruction, etiology of the wound, as well as size of the defect. The following etiologies were most commonly addressed: draining seroma/lymphocele (43), infected wound (54), hematoma/pseudoaneurysm (10), and prophylactic coverage following vascular graft (27). The recurrent infection rate for positively cultured groin infections was 3.8% for the RF versus 26.1% for all other flaps combined (p = 0.03). In a subgroup analysis comparing the RF and SMF, the respective recurrent infection rates were 3.8% versus 19% (p = 0.12). The success rate for definitive closure of a culture-negative, draining groin wound was 90% for RF and 88.5% for the SMF (p = 0.68).
CONCLUSIONS: We present the largest reported series of muscle flaps for the management of complex groin wounds. The flap serves to cover exposed grafts, fill dead space, and improve antibiotic delivery. Therefore, lymphoceles, seromas, and dehisced wounds can be appropriately managed with either an SMF or RF so long as the available muscle is of adequate bulk for the given amount of dead space. In the context of groin wound infections, the RF has demonstrated superior outcomes. Our outcomes-based analysis has led to an algorithmic approach that is described in Figure 1. This study demonstrates that tailoring muscle flap selection to both wound size and etiology will lead to the best outcome. 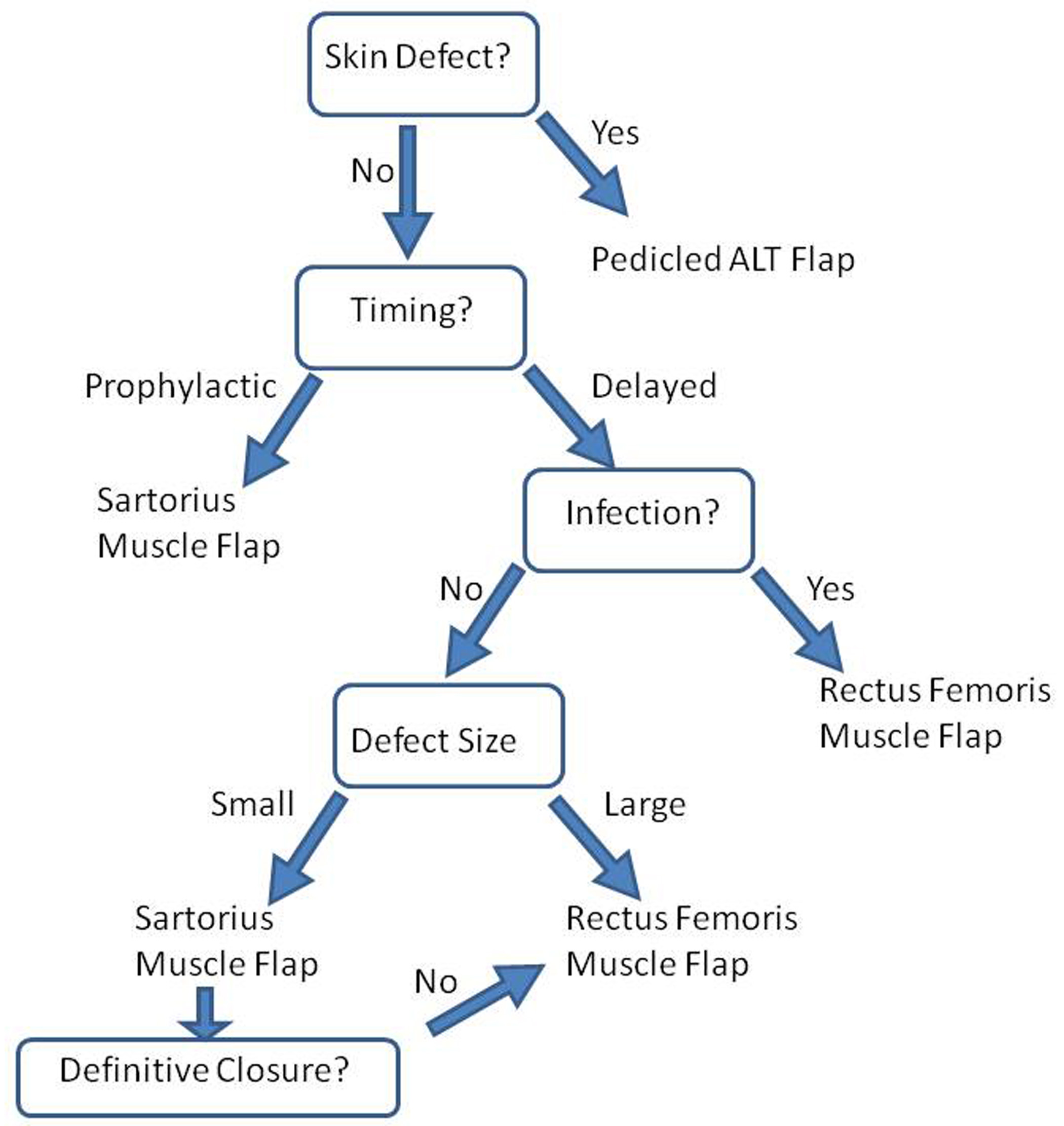
Back to 2011 Program
|