|
|
 |
Back to 2011 Posters
Mathematical Modeling and Frequency Gradient Analysis of Cellular and Vascular Invasion into Integra® and Strattice®: Towards Optimal Design of Tissue Regeneration Scaffolds
Alyssa J. Reiffel, MD1, Ying Zheng, PhD2, Peter W. Henderson, MD, MBA1, Yoann H. Millett, BA1, Lawrence J. Bonassar, PhD3, Abraham D. Stroock, PhD2, Jason A. Spector, MD, FACS1.
1Weill Cornell Medical College, New York, NY, USA, 2Cornell University, School of Chemical and Biomolecular Engineering, Ithaca, NY, USA, 3Cornell University, Department of Biomedical Engineering, Sibley School of Mechanical and Aerospace Engineering, Ithaca, NY, USA.
BACKGROUND: Rapid and effective vascularization via host cell invasion is essential for integration of acellular tissue replacement scaffolds. While the two commercially available products Strattice® and Integra® products are commonly used in clinical practice, they differ significantly in their production and composition. To date, there have been no studies directly comparing the rate and extent of host cell invasion and vascularization of these scaffolds. As such, we designed a study to rigorously and quantitatively evaluate the relative rates of invasion and vascularization of these different acellular scaffolds in a murine model of graft incorporation.
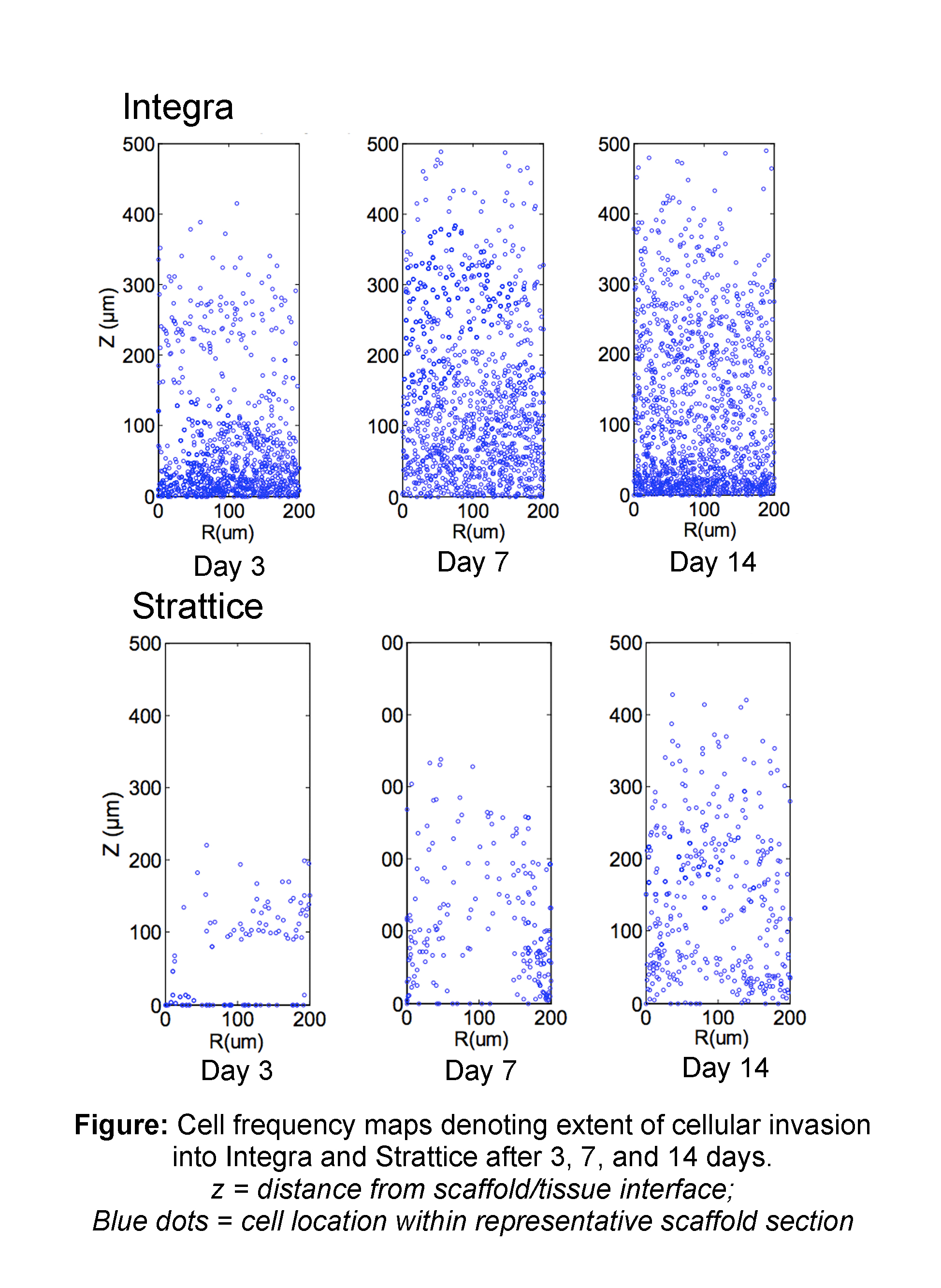
METHODS: Integra® and Strattice® were implanted subcutaneously in the dorsa of C57BL/6 mice, harvested after 3, 7, or 14 days, and stained with H&E, DAPI, and immunohistochemical stains for CD31 and α-smooth muscle actin (α-SMA). Exponential decay equations of the form y=a*(1-b)^x describing cellular invasion through each layer were fit to each material/time point. Differential mean cell densities (representing cellular invasion density as a function of depth within the scaffold, “z”) were extrapolated from DAPI images by quantifying nuclei/unit area in the z-direction for 15 sections of each material. Cell frequency maps (an alternative method of evaluating invasion depicting cellular location in an orthogonal plane) were extracted from DAPI images by translating the center of each nucleus into a matrix of coordinates and combining 15 such matrices of 3 templates for each material/timepoint.
RESULTS: Qualitative analyses demonstrated diffuse and extensive cellular infiltration into Integra® by 3d, increasing over the 2-week period. Invasion of Strattice® was sparse, even after 14d. CD31 immunohistochemistry revealed blood vessel formation within Integra® by 14d. However, there was no perivascular α-SMA positivity, suggesting these blood vessels were immature. There was no analogous vascularization in Strattice®. Mean decay equations for Integra® and Strattice® were y=76.3(0.59)^x and y=75.5(0.33)^x, respectively. Strattice® grafts demonstrated a greater decay rate “b” at all timepoints, translating into a steeper decline of each curve with increasing layer depth, and correlating with the decreased penetration of cells into the bulk of the Strattice® matrix. Cell density measurements showed that at all time points, Integra® manifested a greater density and depth of cellular invasion as compared with Strattice®. Specifically, the number of invading cells within Integra® decreased slightly from day 3 to day 7 and rebounded to the greatest value by 14d. In contrast, the cellular invasion profile of Strattice® did not change considerably over the 2-week period. This finding was confirmed by cell frequency mapping (Figure).
CONCLUSIONS: These data confirm empiric clinical observations that Integra® is more rapidly and efficiently vascularized than Strattice® when placed in a suitable host bed. Furthermore, the presence of a remnant microvasculature template is not sufficient for effective cellular and vascular ingrowth into an artificial tissue construct. These findings provide further insight into means of improving future tissue replacement products to elicit more rapid host cellular invasion and vascular incorporation. 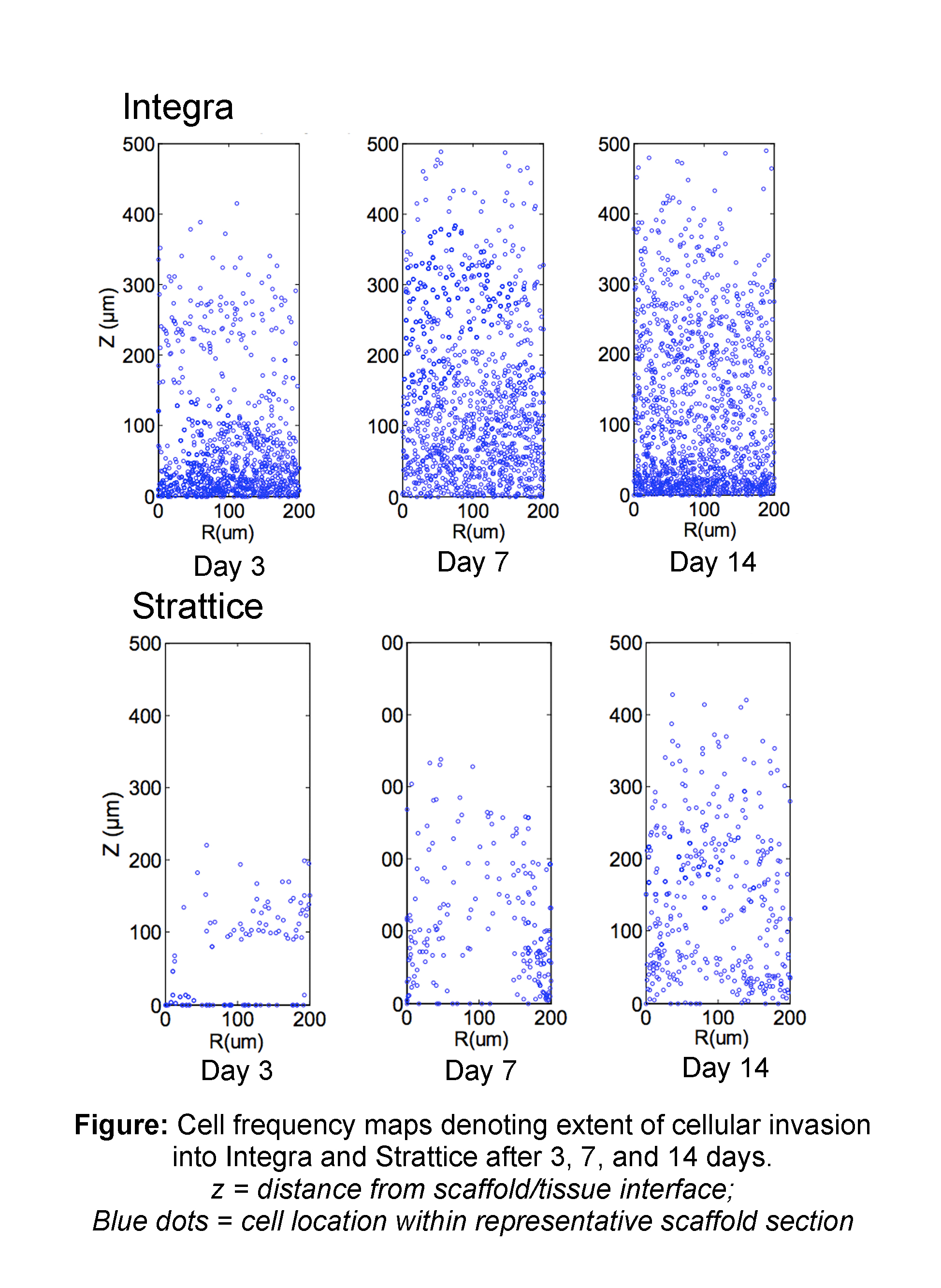
Back to 2011 Posters
|