|
Back to Annual Meeting Program
Does Conventional Posterior Vault Remodeling Alter Endocranial Morphology in Patients With True Lambdoid Synostosis?
River M. Elliott, MD1, James M. Smartt, Jr., MD2, Jesse A. Taylor, MD1, Scott P. Bartlett, MD1.
1University of Pennsylvania, Philadelphia, PA, USA, 2University of Washington, Seattle, WA, USA.
BACKGROUND: True lambdoid synostosis (TLS) is a rare condition with a consistent calvarial
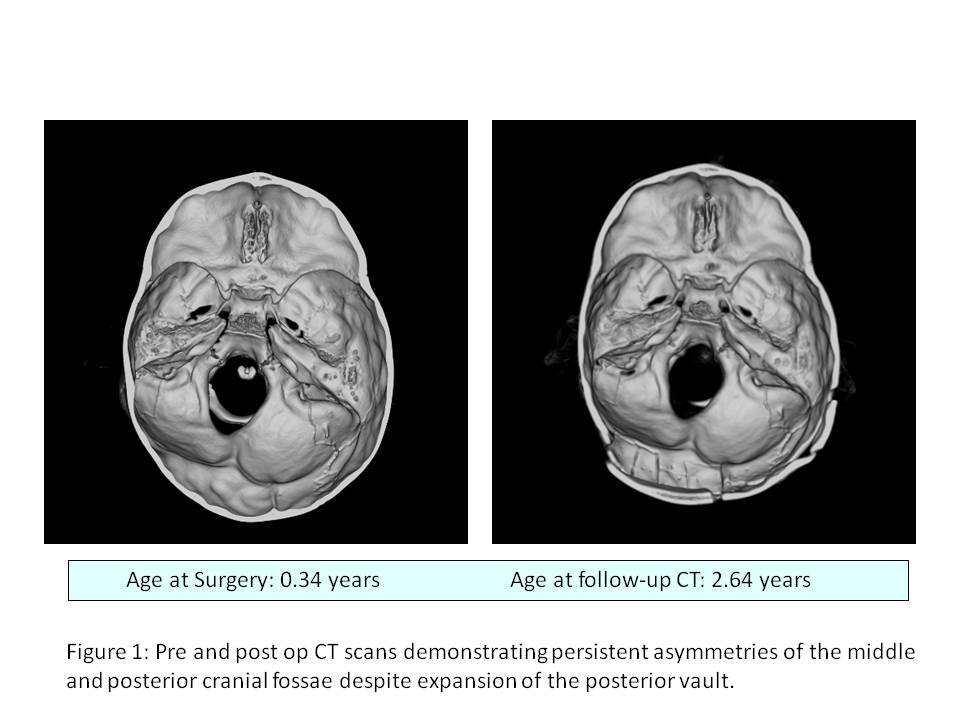
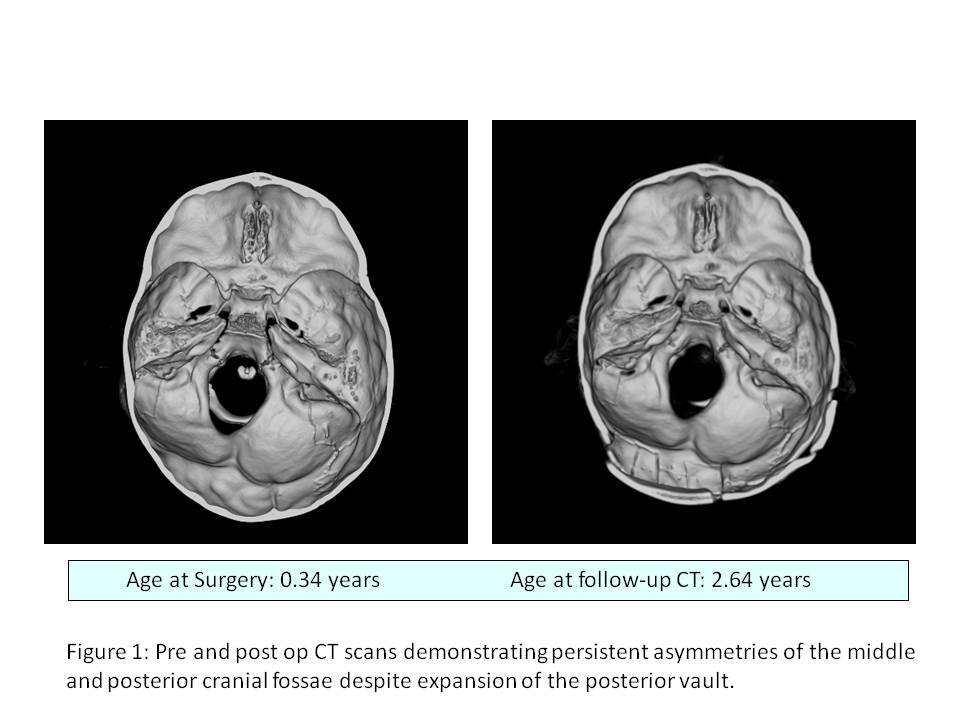
morphology that includes occipital flattening, an ipsilateral occipitomastoid prominence, and a contralateral hemifacial deficiency that minimally improves with surgery. Prior studies at our institution have demonstrated that dysmorphic middle and posterior cranial fossae lead to a craniofacial scoliosis characteristic of the lambdoid phenontype. We hypothesize that these endocranial features persist following surgery, causing the persistent postoperative hemifacial deficiency seen in these patients.
METHODS: Using a TeraRecon Aquarius Workstation, three-dimensional anthropometric measurements were made on pre and post-operative CT scans of patients with TLS (n=5). Quantitative analysis was performed on the following features: middle cranial fossa area (MCF), anterior cranial fossa area (ACF), posterior fossa deflection angle (PFA), petrous ridge angle (PRA), temperomandibular joint angle (AFA), and external auditory meatus angle (EAMA). The results were analyzed using a two-tailed t-test.
RESULTS: Patients underwent conventional posterior vault remodeling at a mean age of 1.33 years (range 0.34-4.44 years). Post operative CT scans were obtained a mean of 1.82 years following surgery (range 0.006-3.11 years). Following surgery, patients with TLS demonstrated an unchanged PFA (p=0.76) with persistent deviation of the posterior cranial fossa toward the affected side. The ACF remained symmetrical after surgery (p=0.212), however the contralateral MCF remained enlarged relative to the ipsilateral side (p=0.003). Moreover, the contralateral middle cranial fossa became significantly more retrodisplaced, as measured by the PRA (p=0.021) while the ipsilateral PRA remained unchanged (p=0.95). Significant asymmetries also remained with respect to ear position (as measured by EAMA, p=0.037). The position of the TMJ was not statistically different between sides either before (p=0.24) or after surgery (p=0.07).
CONCLUSIONS: Traditional methods of treating patients with TLS may effectively restore calvarial shape, however they do not significantly alter the dysmorphic features seen in the cranial base. Specifically, preoperative asymmetries in the middle and posterior cranial vault remain unchanged following surgery. While the ipsilateral middle cranial fossa maintains a stable position postoperatively, retrodisplacement of the contralateral middle cranial fossa progressively worsens. These findings likely explain why a contralateral hemifacial deficiency persists in these patients despite surgical intervention. These data suggest that future operative techniques should be targeted toward the correction of the endocranial deformity as well as the posterior calvarial vault.
Back to Annual Meeting Program
|