|
|
 |
Back to Annual Meeting Program
The Clinical Role of Intraoperative Core Temperature In Free Tissue Transfer
J. Bradford Hill, M.D.1, Kevin W. Sexton, M.D.1, Gabriel A. Del Corral, M.D.1, Ashit Patel, MBChB, MRCS2, Oscar D. Guillamondegui, M.D., M.P.H.1, Jesse M. Ehrenfeld, M.D., M.P.H.1, R. Bruce Shack, M.D.1.
1Vanderbilt University, Nashville, TN, USA, 2Albany Medical Center, Albany, NY, USA.
BACKGROUND: Lengthy microvascular procedures risk patients of hypothermia, yet no existing study has evaluated the overall impact of core temperature on patient and flap morbidity. While hypothermia may contribute to complication, warming measures are challenged by reports that intraoperative hypothermia may improve anastomotic patency.
METHODS: A retrospective review included all free flaps performed by plastic surgeons at an academic medical center from December 2005 to December 2010. Intraoperative core temperatures were measured by esophageal probe and median values recorded over five-minute intervals yielded a case mean (Tavg), maximum (Tmax) and nadir (Tmin). Outcomes included flap failure, pedicle thrombosis, recipient site infection and complications associated with patient and flap morbidity. Analysis utilized Student’s T-test, Fisher’s exact test, Probit and logistic regression.
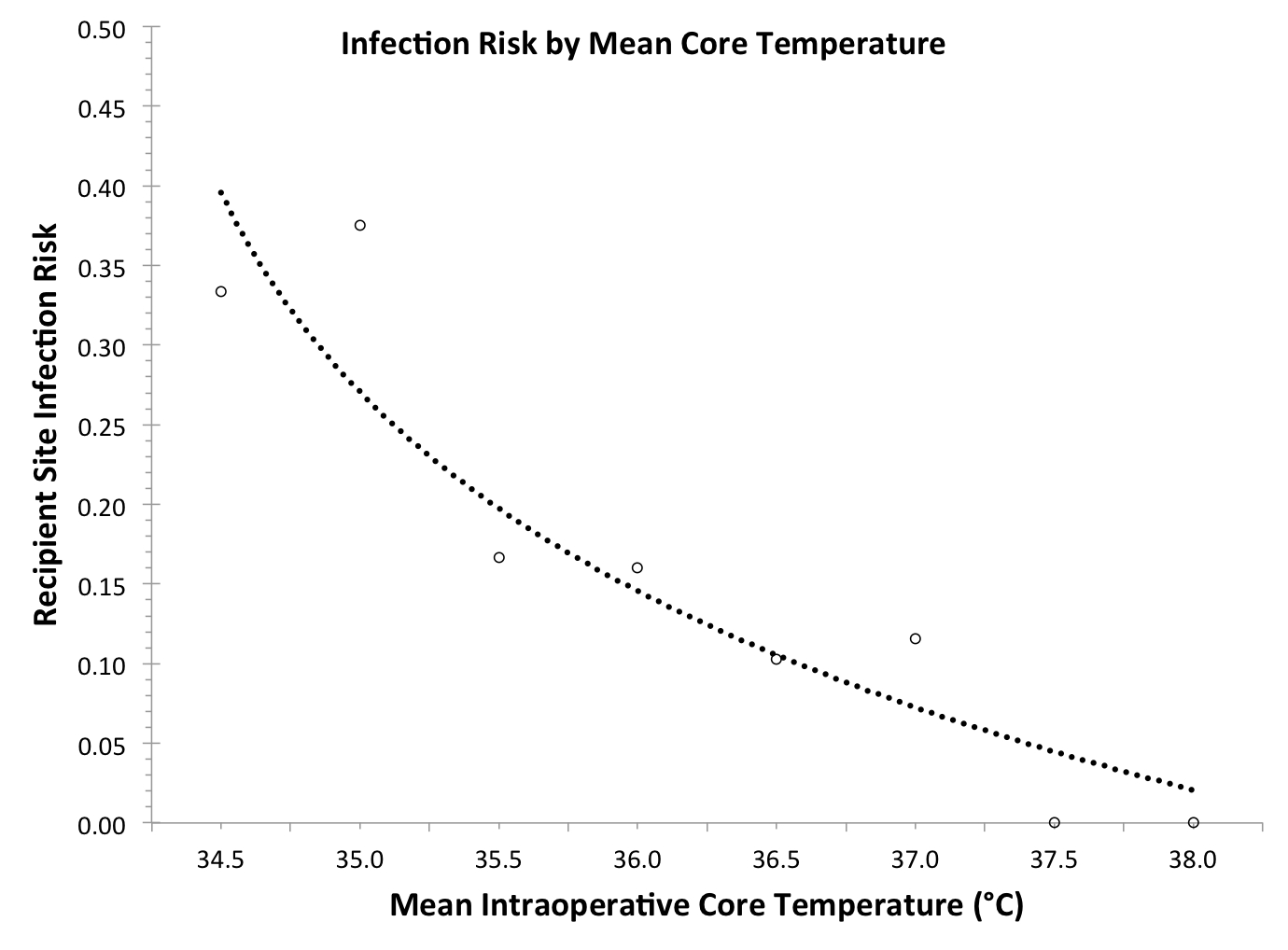
RESULTS: Of 156 consecutive free tissue transfers, the median Tavg, Tmax and Tmin were 36.5°, 37.1°, and 35.8°C, respectively. The flap failure rate was 7.7%[12/156] and pedicle thrombosis occurred in 9[6%] cases. Core temperatures did not associate with overall flap failure or pedicle thrombosis but recipient site infection occurred in 21[13%] patients who had significantly lower mean core temperatures (Tavg = 36.0°C, p < 0.01). Lower Tavg and Tmax significantly predicted recipient site infection (p < 0.01, p < 0.05, respectively) [Figure 1]. Cut-point analysis revealed significant increases in recipient site infection risk at Tavg < 37.0°C (p = 0.026) and Tmin ≤ 34.5°C (p = 0.020).
CONCLUSIONS: Intraoperative hypothermia posed significant risk of recipient site infection with no benefit in anastomotic patency. These findings support diligent maintenance of normothermia in free tissue transfer.
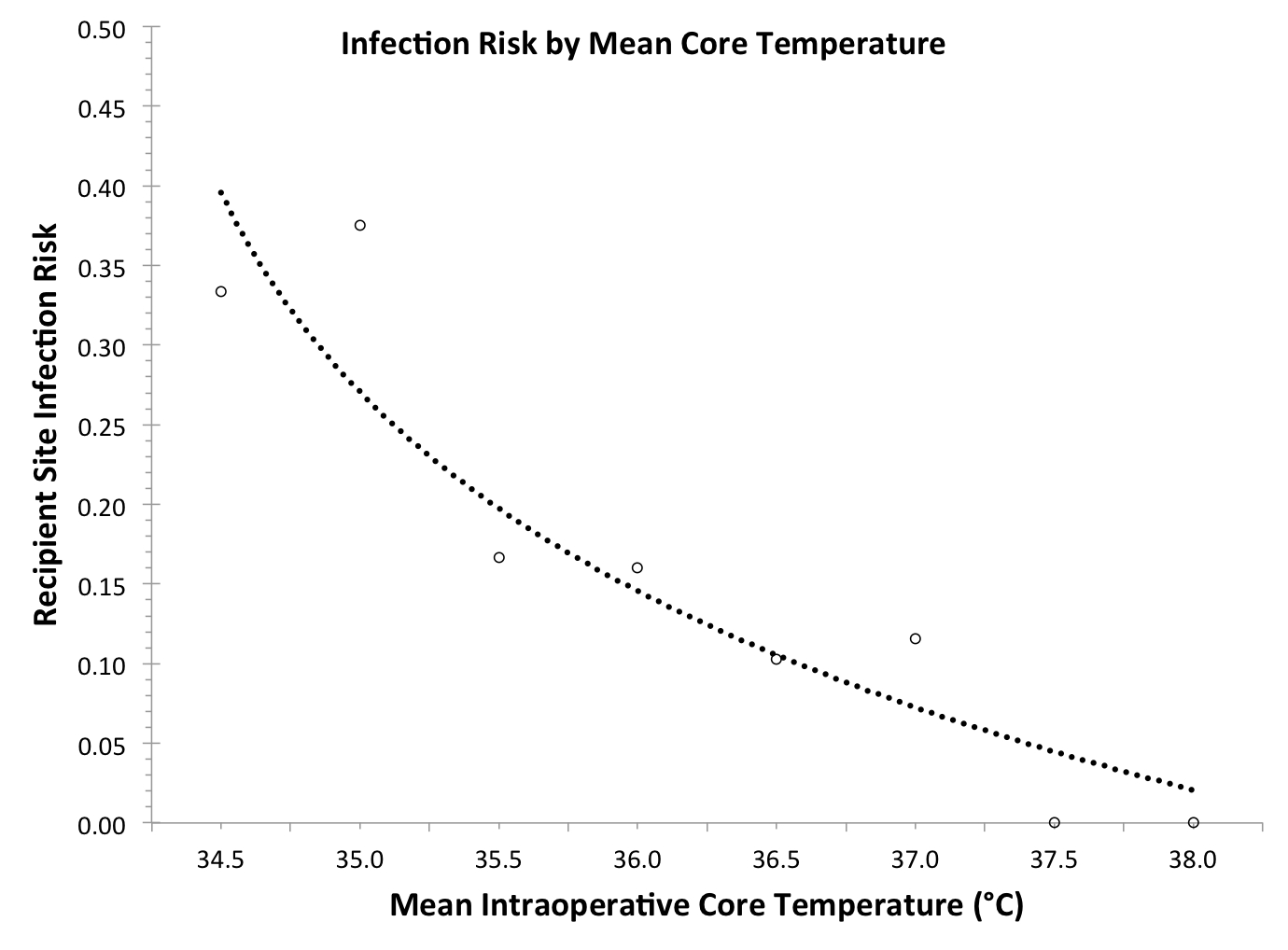
Figure 1. Infection risk is illustrated by mean core temperature. Observed values are represented by circles and the trend line is predicted risk. Probit analysis provided support for causality via a statistically significant exposure-response relationship (p < 0.01).
Back to Annual Meeting Program
|