|
|
 |
Back to Annual Meeting
Utility of Tissue Expansion in Pediatric Phallic Reconstruction: A 10-Year Experience
Danielle H. Rochlin, BA1, Karl Zhang, MD2, John P. Gearhart, MD3, Ariel Rad, MD, PhD1, Alex Kelamis, MD1, Ranjiv Mathews, MD3, Richard J. Redett, MD1.
1Department of Plastic and Reconstructive Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, USA, 2Department of Radiology, State University of New York Downstate Medical Center, Brooklyn, NY, USA, 3Department of Urology, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
BACKGROUND: Males with complex penile anomalies such as hypospadias and epispadias often undergo several reconstructive procedures to achieve successful cosmetic and functional outcomes. Multiple surgical revisions can leave a paucity of healthy, unscarred skin for further surgical reconstruction. Although a variety of graft and local flap options exist, these are associated with high complication rates, including wound healing problems, incongruity of skin color, recurrent fistula, and/or urethral stricture. Local skin expansion can provide an abundance of well-vascularized, hairless, pigment- and texture-matched skin for penile reconstructive procedures. We report here the largest experience with the use of tissue expansion for phallic reconstruction in males with congenital penile anomalies.
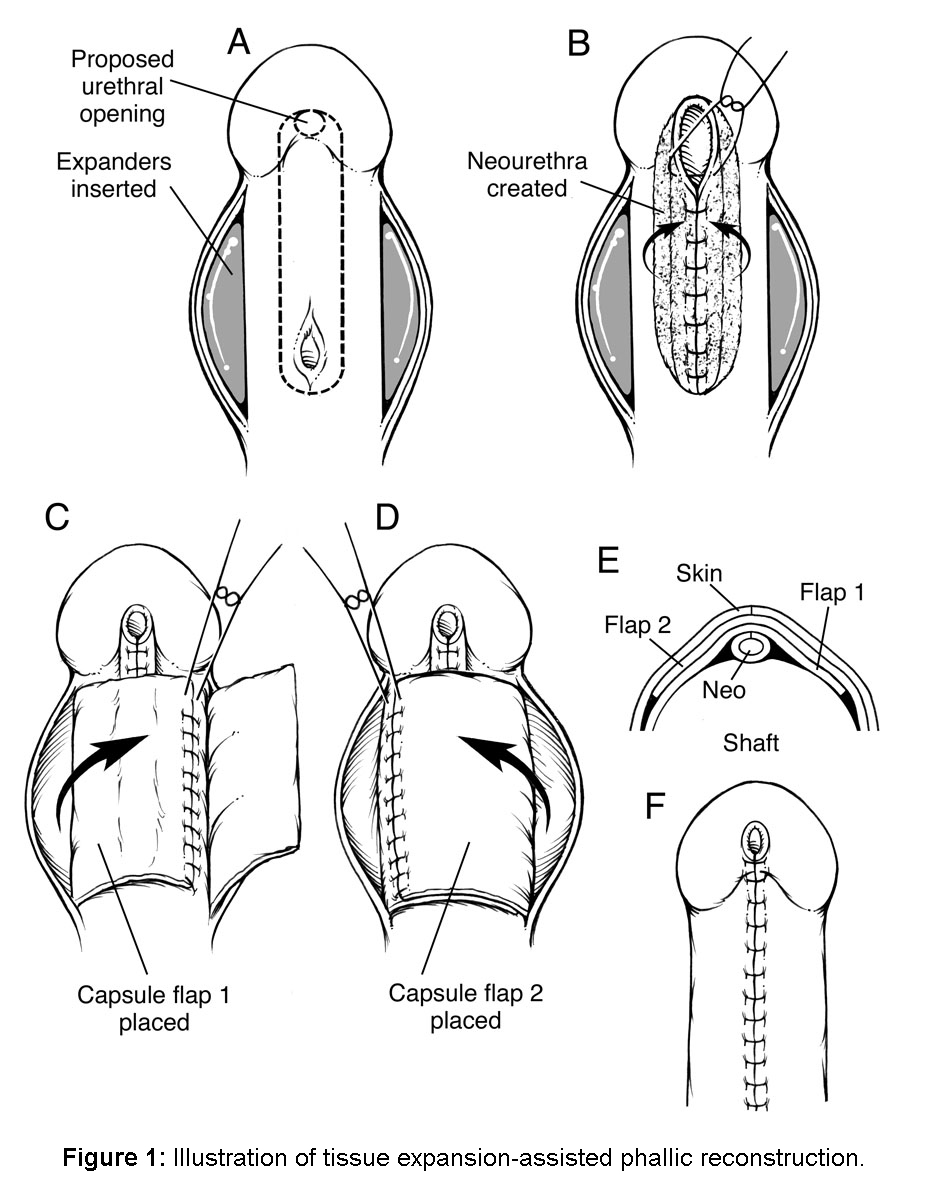
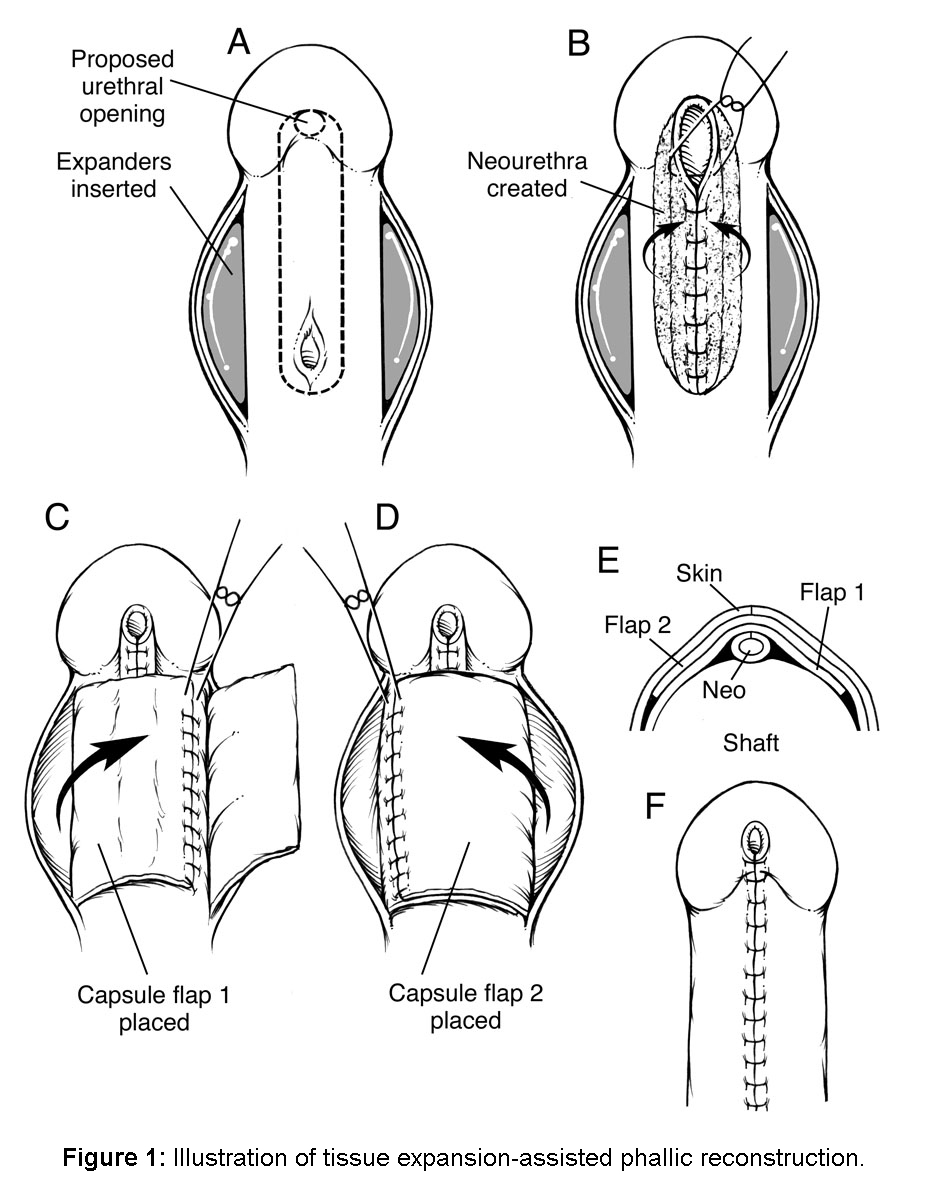
METHODS: We reviewed our experience with tissue expansion in patients that had failed multiple prior procedures for phallic reconstruction of a congenital penile anomaly. Eighty males (mean age of 11.9 years) with underlying diagnoses of hypospadias (n=42) and epispadias (n=38) formed the cohort for the study. All patients had undergone at least one prior failed reconstructive operation. Indications for tissue expansion included scarcity of penile skin in the setting of recurrent urethral stenosis, urethrocutaneous fistula, residual hypospadias or epispadias, and/or chordee. One or two expanders were placed under the skin of the shaft of the penis (Figure 1), and removed at the time of phallic reconstruction in uncomplicated cases.
RESULTS: Average time between tissue expander placement and reconstruction was 10.9 weeks. Mean follow-up time was 25.3 months. Eighteen patients (22.5%) had a single tissue expander placed and 62 (77.5%) had dual tissue expander implants. Complications during tissue expansion included infection ± extrusion (n=10), expander leak ± extrusion (n=8), isolated extrusion (n=18), migration (n=3), and hematoma (n=1). Overall, 22 patients (27.5%) had at least one expander removed and 46.9% of these expanders were replaced. Seventy-six patients (95.0%) were able to undergo successful expansion and had adequate tissue for reconstruction. Thirty-nine patients had a successful outcome after initial reconstruction and 25 achieved a successful result after further reparative and/or reconstructive operations, yielding an overall success rate of 80.0%. Twelve patients experienced failure of the reconstruction due to residual fistula (n=5), abnormal urethral location (n=4), wound healing problems (n=2), or recurrent stricture (n=1).
CONCLUSIONS: Tissue expansion is a useful tool with an acceptable rate of complications for penile reconstruction in patients who have failed prior surgical reconstruction and are left with a paucity of residual skin. Outcomes with tissue expansion-assisted reconstruction will continue to improve as surgeons gain experience using this advantageous technique in phallic reconstruction.
Back to Annual Meeting
|