|
Back to Annual Meeting
Vascularized Thoracodorsal and Lateral Thoracic Artery-Based Lymph Node Transfer for the Treatment of Lymphedema: Technique and Case Series
Erez Dayan, M.D., Mark L. Smith, M.D., Mark Sultan, M.D., William Samson, M.D., Joseph H. Dayan, M.D..
Beth Israel Medical Center, New York, NY, USA.
BACKGROUND:
Vascularized groin lymph node transfer has been described as a successful treatment for lymphedema. However, patients with bilateral lower extremity lymphedema may not be candidates, and the short pedicle may not be ideal if the recipient site requires greater pedicle length. Transfer of axillary lymph nodes draining the chest wall has been performed but there is no literature on the technical details of this procedure. We present a case series and technique for vascularized axillary lymph node transfer using reverse lymphatic mapping to minimize the risk of lymphedema in the upper extremity.
METHODS:
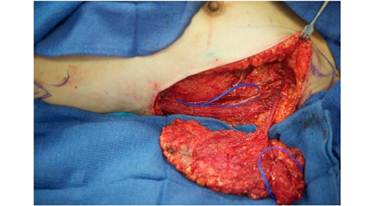
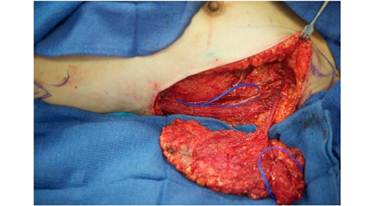
Four patients underwent axillary lymph node transfer between October 2011 and June 2012: two patients with lower extremity lymphedema and 2 with upper extremity lymphedema. Reverse lymphatic mapping using technetium injection into the upper extremity and indocyanine green into the chest wall was used to avoid harvesting lymph nodes draining the upper limb and to facilitate chest wall lymph node harvest. Donor lymph nodes were harvested based on the thoracodorsal artery in 2 cases and based on both the thoracodorsal and lateral thoracic arteries in the remaining 2 cases. A thoracodorsal artery perforator skin paddle was included in 3 of the 4 cases. Intravenous indocyanine green and SPY evaluation was used to confirm perfusion of lymph nodes following anastomosis. Video and technical details will be illustrated.
RESULTS:
All patients had viable free flap transfers with satisfactory perfusion of the lymph nodes confirmed by intraoperative SPY evaluation. There were no postoperative complications and no observed lymphedema in the limb adjacent to the lymph node harvest donor site. Our first patient experienced a significant reduction in upper extremity limb volume as illustrated in the attached figures. Long-term follow-up on volumetric data and quality of life will be provided at the time of the meeting with a follow-up range of 7 - 15 months.
CONCLUSIONS:
Axillary lymph node transfer may be a useful alternative to groin lymph nodes and provides a long pedicle which may be preferable in a severely radiated or hostile recipient environment.
Back to Annual Meeting
|