|
|
 |
Back to Annual Meeting
Optimizing patient selection in Abdominal Contouring Surgery following Massive Weight Loss: Analysis of 4,925 patients undergoing Abdominoplasty with and without Concurrent Hernia Repair.
Pieter G. L. Koolen, M.D.1, Ahmed M. S. Ibrahim, M.D.1, Kuylhee Kim, M.D.1, Hani H. Sinno, M.D., MEng2, Samuel J. Lin, M.D.1.
1Harvard Medical School/Beth Israel Deaconess Medical Center, Boston, MA, USA, 2McGill University, Montreal, QC, Canada.
Background
Bariatric surgery has become an increasingly popular tool to lose weight. Although massive weight loss following this procedure has numerous health benefits, it also presents with negative effects due to the excess skin and subcutaneous tissue that result. There has been a significant rise in the number of abdominal contouring surgeries (ACS) performed to address this issue. However, resection of excess abdominal skin in these patients carries the risk of multiple postoperative complications. Given the excellent intra-operative exposure of the abdominal wall during ACS, concurrent ventral/umbilical/inguinal hernia repair (HR) is often performed. We evaluated the incidence of postoperative complications following ACS with or without concurrent hernia repair in a nationally validated, multicenter database and identified specific risk factors that predisposed to these complications.
Methods
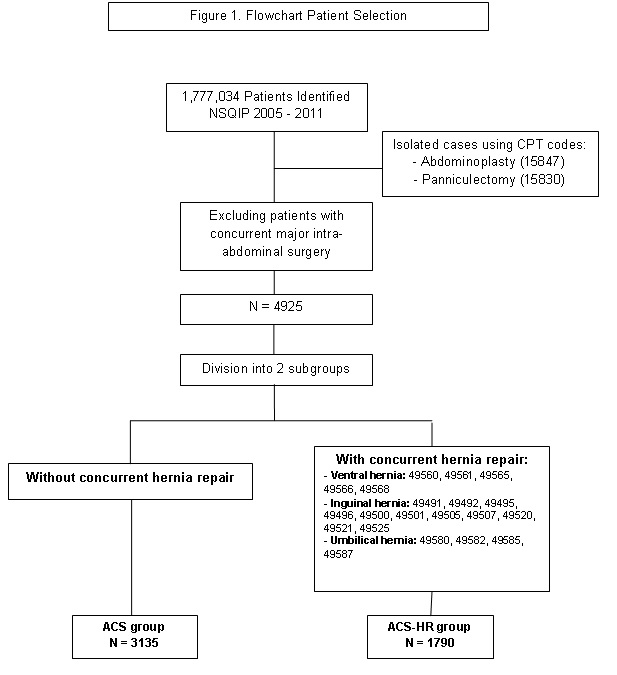
A prospective, multi-institutional study of patients undergoing abdominal contouring surgery with or without concurrent hernia repair was performed using the American College of Surgeon’s National Surgical Quality Improvement Program from 2005 to 2011. The incidence of postoperative complications was determined with specific emphasis on wound related complications. A logistical regression model was developed to predict the influence of demographics and co-morbidities on postoperative outcomes.
Results
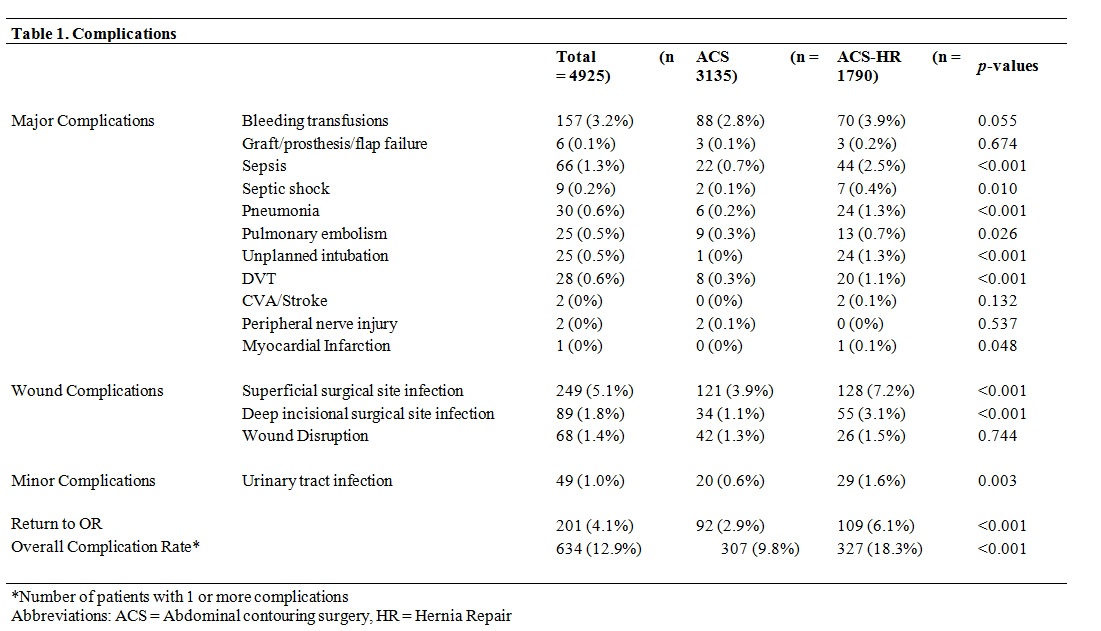
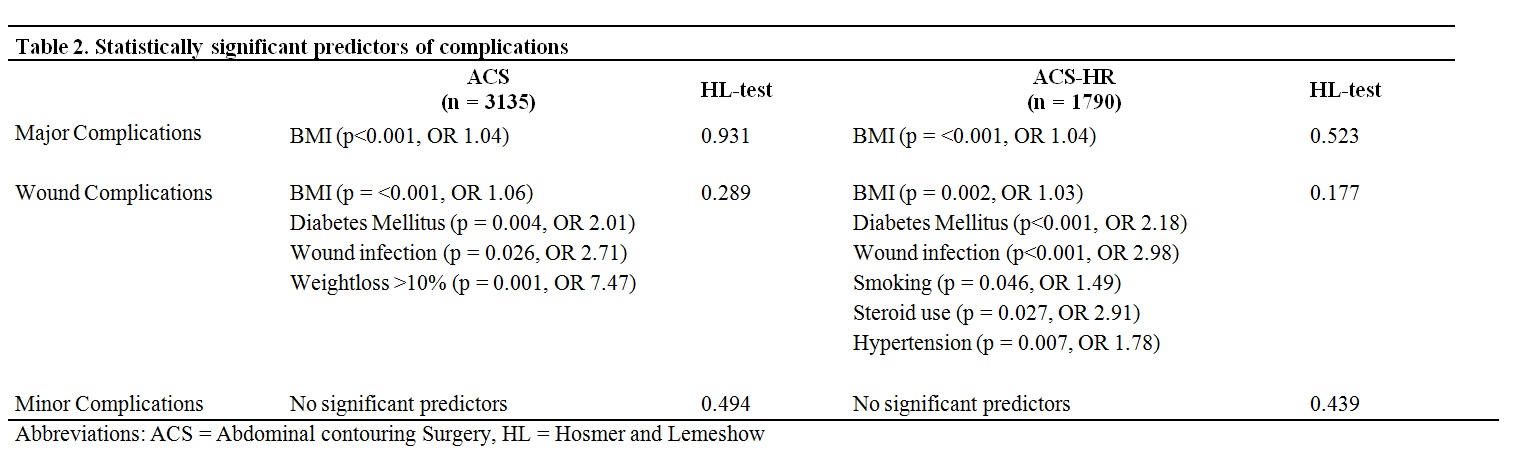
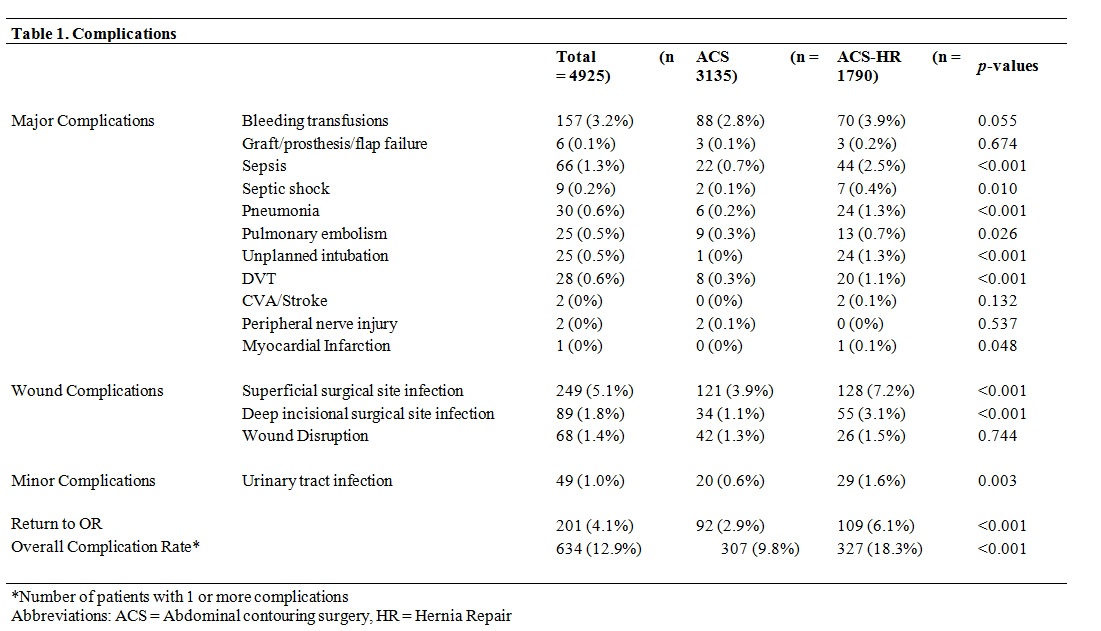
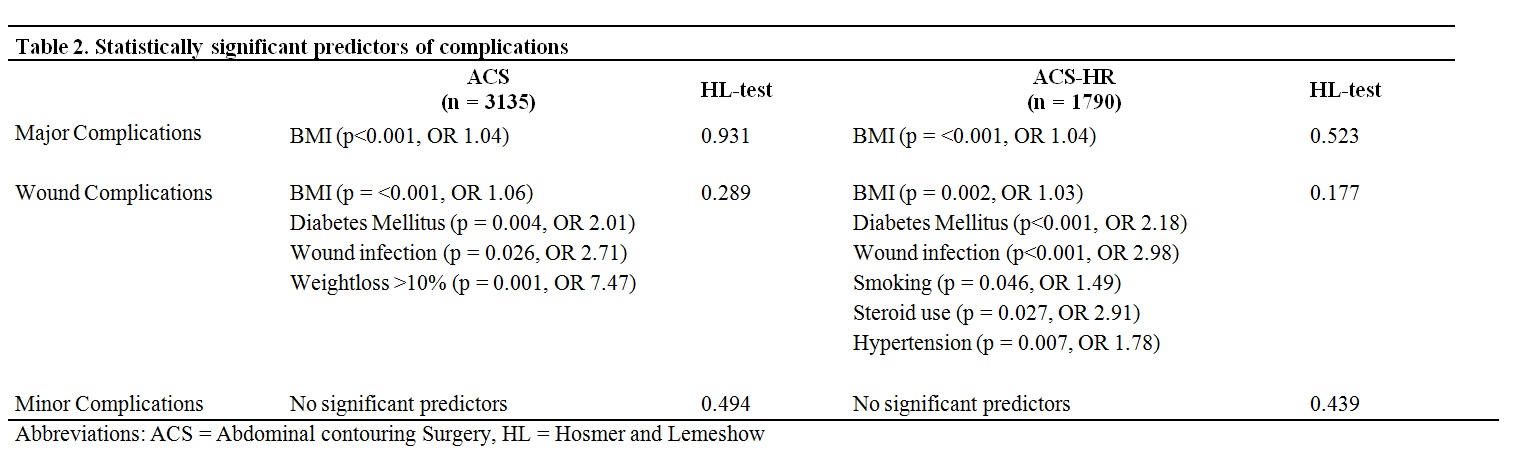
After excluding patients who had undergone concomitant procedures involving major intra-abdominal surgery, a total of 4,925 patients were identified using Current Procedural Codes for abdominoplasty and/or panniculectomy. Of these, 36.3% (n=1,790) received a simultaneous hernia repair (ACS-HR) and 63.7% (n=3,135) did not (ACS). Patients undergoing ACS-HR had more co-morbidities at baseline. Furthermore, overall complication rate in the ACS-HR group was significantly higher (18.3% vs. 9.8%, p<0.001). Elevated BMI served as predictor for major and wound complications in both groups, especially for superficial (ACS odds ratio (OR): 1.05; ACS-HR OR: 1.22) and deep (ACS OR: 1.06; ACS-HR OR: 1.02) surgical site infections. Diabetes (ACS OR: 2.01; ACS-HR OR: 2.18) and previous wound infection (ACS OR: 2.71; ACS-HR OR: 2.98) were found to be predictors for wound complications in both groups. Smoking, chronic steroid use and hypertension served as predictors for wound complications in the ACS-HR group only (OR: 1.49, 2.91, and 1.78 respectively).
Conclusions
Patients undergoing ACS-HR have a higher postoperative complication rate which can associated with a worse general condition. These patients were more likely to have a history of hypertension, smoking, and chronic steroid use which all served as predictors for negative outcomes. These factors should be carefully considered when assessing the surgical protocol for a patient undergoing ACS emphasizing the need for surgeons to be meticulous in their patient selection process.
Back to Annual Meeting
|