|
Back to Annual Meeting
Does Flap Reconstruction Make a Difference in Complications Following Laryngopharyngectomy? Analysis of the NSQIP Database
Kuylhee Kim, M.D.1, Ahmed M. S. Ibrahim, M.D.1, Pieter G. L. Koolen, M.D.1, Hani H. Sinno, M.D., MEng2, Samuel J. Lin, M.D.1.
1Harvard Medical School/Beth Israel Deaconess Medical Center, Boston, MA, USA, 2McGill University, Montreal, QC, Canada.
BACKGROUND:
For the laryngopharyngeal defect following ablation of advanced cancer, surgeons are faced with the challenge of minimizing morbidity and mortality in a high-risk population while attempting to achieve adequate functional results. Laryngopharyngeal reconstruction using flaps was adopted for the purpose of restoring continuity to the upper aerodigestive tract, protection of major blood vessels, aiding in primary wound healing, and achieving superior swallowing and speech functions. The aim of our study was to assess the impact of reconstructive procedures on patients undergoing laryngopharyngectomy and to determine whether 30-day postoperative morbidity and mortality varied between patients who underwent flap reconstruction and those that did not.
METHODS:
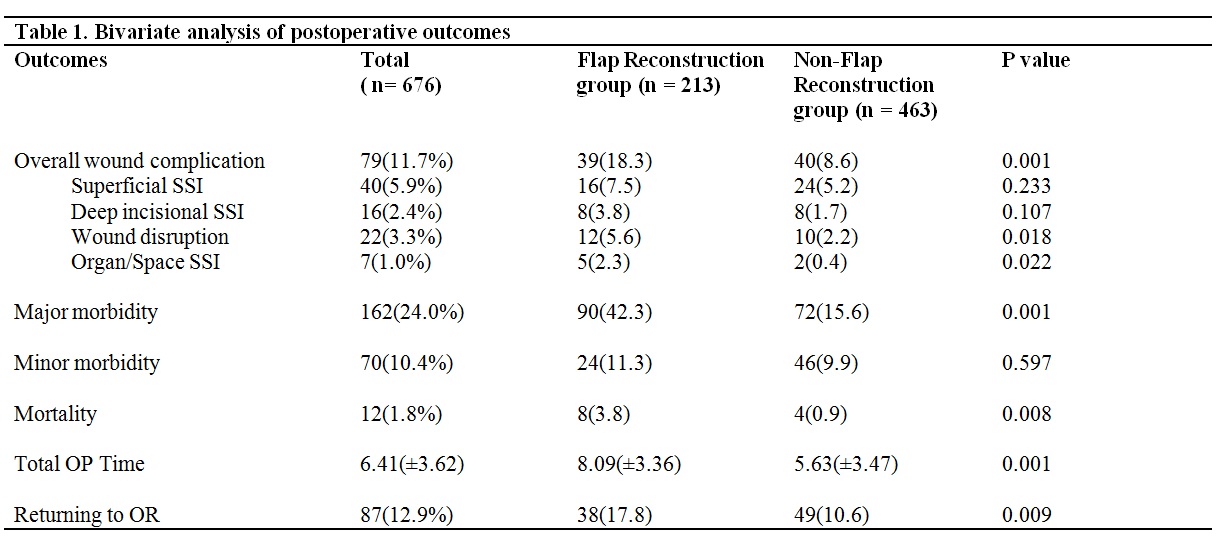
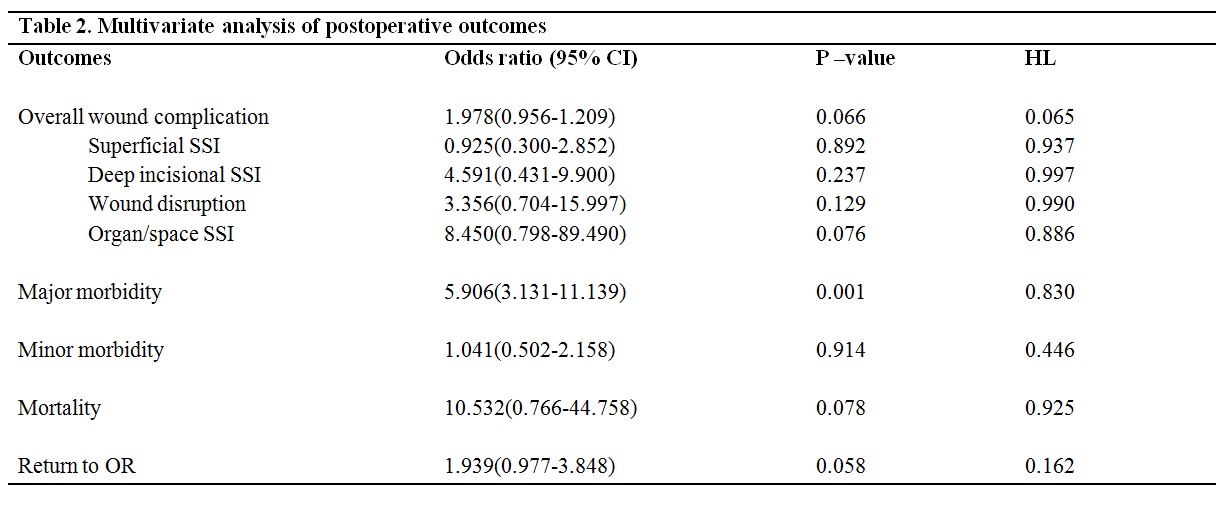
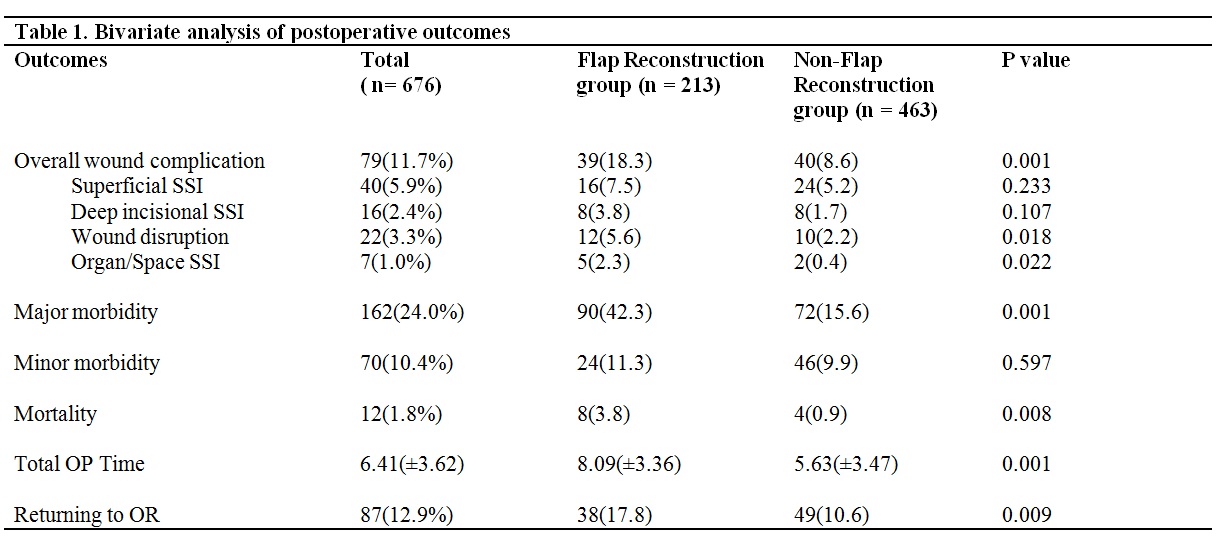
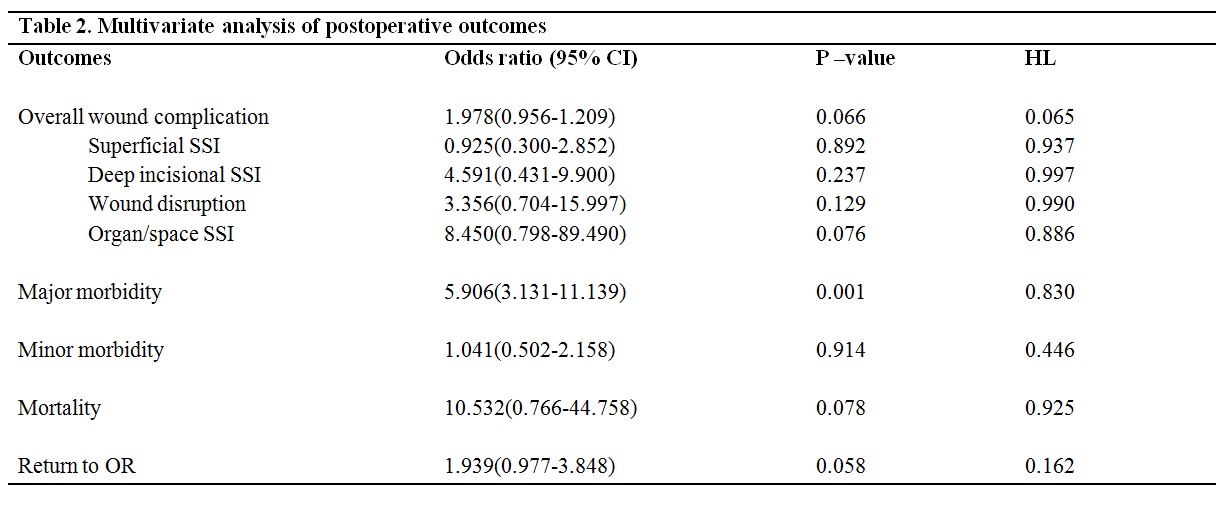
We reviewed the 2005-2011 ACS-NSQIP database to identify patients undergoing laryngectomy and/or pharyngectomy. A bivariate analysis was done to compare preoperative variables and postoperative outcomes between the flap reconstruction group and non-reconstruction group. Chi-square tests were used for categorical variables and t-tests for continuous variables. Multivariate analysis was performed to calculate odds ratio to account for potential confounders. A bivariate screen was used to identify variables that demonstrated significance at a standard p-value using the multivariate regression model.
RESULTS:
676 patients were included in our study; 213 patients received concurrent flap reconstruction whereas 463 did not. After risk adjustment, analyses revealed that there was no statistically significant difference in wound complication, minor morbidity, and mortality between the two groups. The flap reconstruction cohort showed significantly longer operative times (8.09 (±3.36) hours vs. 5.63(±3.47) hours P=0.001) and higher major morbidity rate (OR=5.906, 95% CI: 3.131-11.139, P=0.001).
CONCLUSIONS:
This study is the first comprehensive analysis of flap reconstruction for laryngopharyngeal defects using the ACS-NSQIP registry. Additional measures involved in flap reconstruction are associated with an increase in major morbidity but not mortality. An understanding of these variables may optimize the decision-making process for patients undergoing laryngectomy and/or pharyngectomy.
Back to Annual Meeting
|