|
|
 |
Back to Annual Meeting
Can Laser Assisted Indocyanine Green Angiography Detect Venous Congestion more Reliably than Clinical Assessment in a Rat Venous Occlusion Model?
Ahmed E. Nasser, MD, Mitchell Fourman, MPhil, Robert P. Gersch, PhD, Hsingli Hsi, MS, Breet T. Phillips, MD, Alexander B. Dagum, MD, Mark A. Gelfand, MD, Duc T. Bui, MD.
Stony Brook University Hospital, Stony Brook, NY, USA.
BACKGROUND:
Venous Congestion is the top cause for free flap failure and has an incidence that is four times that of arterial thrombosis. Postoperative diagnosis of a congested flap still relies on clinical observation as the gold standard. Studies have shown that revision of venous anastomosis is more successful in the first 24-48 hours. We hypothesized that in a rat lower limb venous congestion model, Laser Assisted Indocyanine Green Angiography (LAICGA) can detect venous congestion and differentiate between a congested and non-congested limb more reliably than clinical observation.
METHODS:
A severe model of lower limb venous congestion was created by bilateral amputation of the lower extremities of male Sprague Dawley rats weighing 250-300g at the level of the proximal femur while preserving only the femoral artery, femoral vein and femur intact. One limb had the femoral vein occluded at its most distal point (near the inguinal ligament) and was compared to contralateral sham control. Complete venous occlusion was achieved by suture ligature (n=5), whereas partial venous occlusion was achieved by surrounding the vein with a micro-tube (polyethylene or silicon) of varying inner diameter to achieve 75% (n=6), 85% (n=4) and 92% (n=4) occlusion respectively. Approximately 10 minutes after occlusion, pictures of the feet were taken before and after a 10 minute scan using LAICGA. Clinical assessment of the pictures was done by a blinded plastic surgeon to determine the occurrence of occlusion and whether it warranted surgical intervention.
RESULTS:
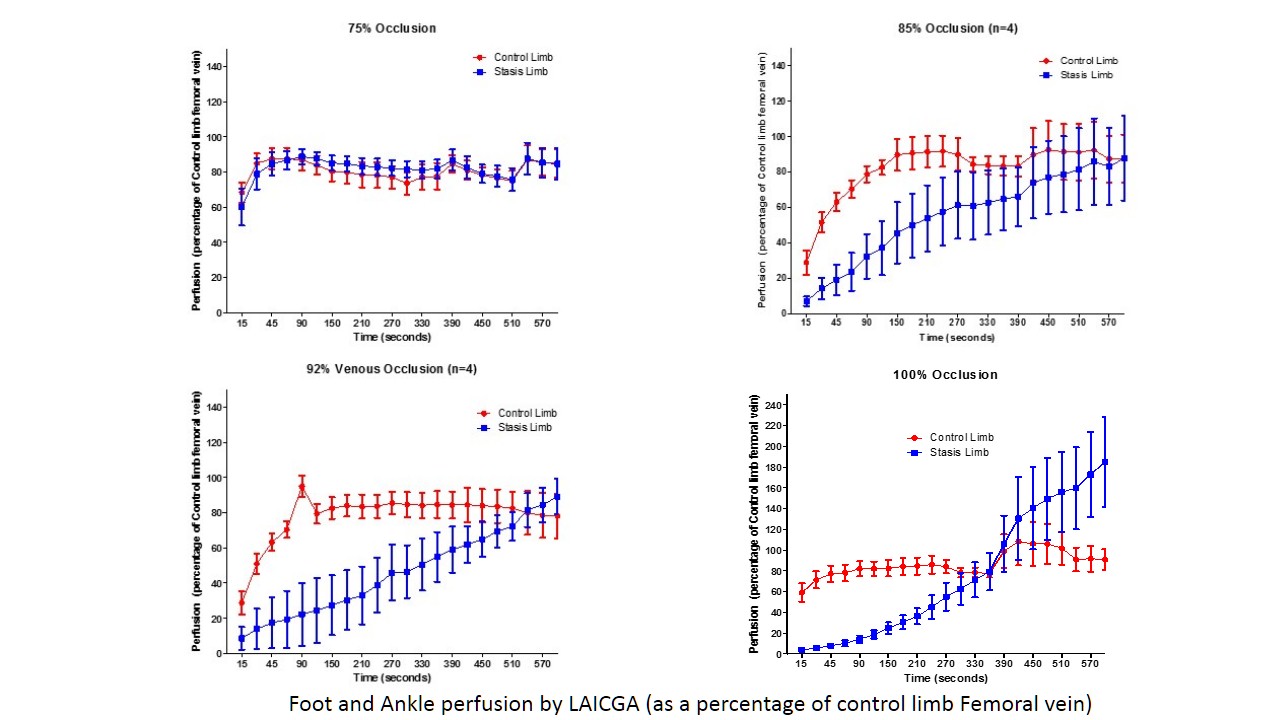
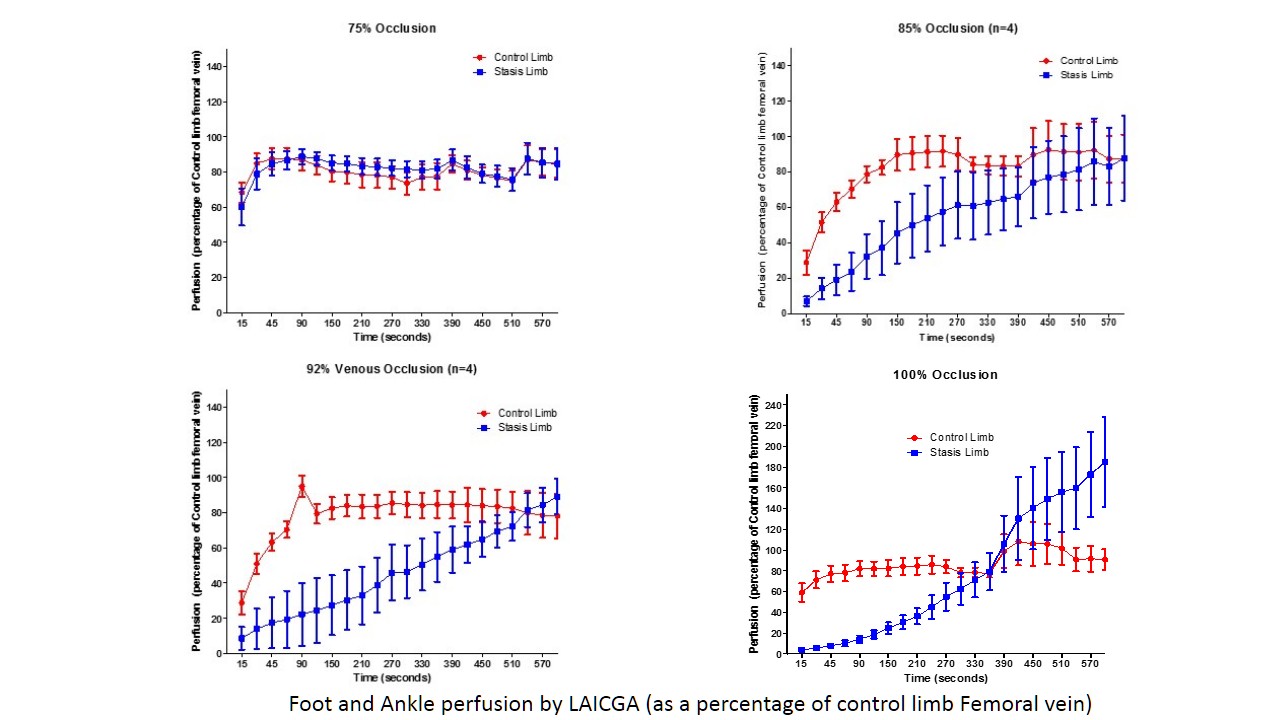
Clinical assessment by the plastic surgeon diagnosed all 5 animals as congested and that all 5 would need surgical intervention in the 100% venous occlusion group. All 4 animals in the 92% group were also diagnosed by the surgeon as congested, but only 3 of the 4 warranted surgical intervention. The 85% group showed 4 of 4 diagnosis rate but only 2 of the 4 were severe enough for intervention. Finally, in the 75% group only 1 of 5 animals (6th animal had no picture) was diagnosed as being congested and it did not warrant intervention. By comparison, LAICGA was able to detect a statistically significant difference in perfusion within the first 2 minutes (12mins from occlusion) in all animals in the 100%, 92% and 85% groups (paired t-test p=0.001, p=0.040 and p=0.030 respectively). LAICGA did not show a difference between limbs in the 75% occlusion group.
CONCLUSIONS:
We demonstrate that LAICGA is able to reliably detect venous congestion in a rat lower extremity model at occlusion rates greater than 75%. At the same levels, clinical judgment detects venous congestion but is less reliable in determining the severity of the congestion. Despite its limitations, our model serves as a basis to further study varying venous occlusion levels, their long term effects and the role of LAICGA in diagnosis.
Back to Annual Meeting
|