|
|
 |
Back to Annual Meeting
Effect of PEMF Regimen on Post-Operative Pain Relief in Breast Reduction Patients
Erin Taylor, B.A.1, Krista Hardy, B.A.1, Arthur Pilla, PhD2, Christine Rohde, MD, MPH1.
1Division of Plastic and Reconstructive Surgery, Columbia University Medical Center, New York, NY, USA, 2Department of Biomedical Engineering, Columbia University, New York, NY, USA.
Background: Non-invasive pulsed electromagnetic field (PEMF) therapy significantly accelerates pain reduction and decreases narcotic requirements after breast reduction (BR) and autologous flap breast reconstruction. PEMF is known to rapidly augment nitric oxide (NO) normally released in injured tissue, which can lead to accelerated pain relief. NO signaling itself is dynamic and self-regulating. Therefore, this study was designed to assess the effect of PEMF regimen on the rate of post-op pain decrease.
Methods: The original BR study was double-blind, randomized, and placebo-controlled (Rohde 2010). This study added two groups of BR patients receiving two different PEMF regimens to be compared with actives in the original study. Pain scores by visual analog scale (VAS) and pain medication use were recorded. The original regimen was 20 min. PEMF every 4 hours (7% duty cycle, n=12), “Q4”. Two additional patient groups were studied, one with a PEMF regimen of 15 min. every 2 hours (12% duty cycle, n=13), “Q2”, and another with a PEMF regimen of 5 min. every 20 minutes (25% duty cycle, n=13), “5/20”. VAS pain scores were measured starting at one hour post-op, and measured until discharge on post-op day 1.
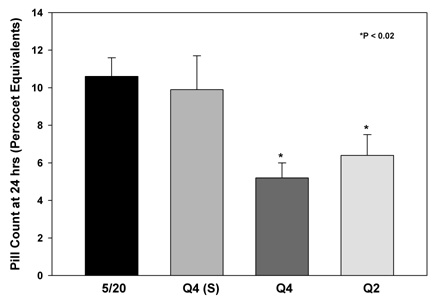
Results: This study found that pain at 12 hrs. post-op, normalized to 1 hr., was 41% and 32% of pain at 1 hr. for Q4 and Q2 regimens, respectively (Fig. 1). In contrast, pain at 12 hrs for 5/20 was 77% of pain at 1 hr., compared to 73% for Q4 shams. The rate of post-op pain reduction was 30% faster for Q2 vs Q4. Pain decreased 2-fold faster for Q4 and Q2 than for 5/20. Concomitantly, post-op narcotic usage was 2-fold higher by 24 hrs for 5/20 compared to Q4 and Q2 regimens and was not different from Q4 shams (Fig. 2).
Conclusions: This study provides evidence that dosing of PEMF therapy is clinically significant. The 5/20 regimen increases NO in the wound bed 2-fold faster than Q2 and 4-fold faster than Q4, which may be large enough to trigger natural negative feedback mechanisms controlling the rate of increase of NO in a wound. The dose effect of regimen reported here is supported by results from human fibroblast cultures, which show PEMF-enhanced NO release can be blocked by PEMF doses high enough to affect negative feedback mechanisms for NO.
Rohde C, Chiang A, Adipojou O, Casper D, Pilla AA. “Effects of Pulsed
Electromagnetic Fields on IL-1β and Post Operative Pain: A Double-Blind, Placebo-Controlled Pilot Study in Breast Reduction Patients.” Plast Reconstr Surg. 2010, 125: 1620-1629.
Fig 1: Effect of PEMF regimen on post-op pain reduction.
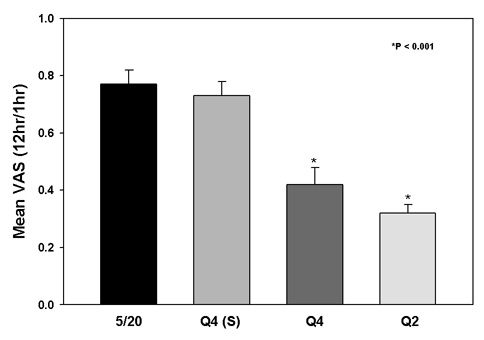
Fig 2: Effect of PEMF regimen on post-op narcotic requirements (Percocet equivalents)
Back to Annual Meeting
|






