|
|
 |
Back to Annual Meeting
Risk Analysis and Stratification of Surgical Morbidity following Immediate Breast Reconstruction (IBR)
John P. Fischer1, Ari M. Wes, BA1, Charles T. Tuggles, III, MD2, Joseph M. Serletti, MD1, Liza C. Wu, MD1.
1University of Pennsylvania, Philadelphia, PA, USA, 2Yale School of Medicine, New Haven, CT, USA.
Background:
Surgical complications following breast reconstruction can be associated with significant morbidity, dissatisfaction, and cost. We use the ACS-NSQIP datasets from 2005-2011 to derive predictors of morbidity and to stratify risk following immediate breast reconstruction (IBR).
Methods:
Surgical complications following implant and autologous reconstruction were assessed using the ACS-NSQIP 2005-2011 datasets. Patient demographic and clinical characteristics as well as operative factors were associated with the likelihood of experiencing a surgical complication. A "model cohort" of 12,129 patients was randomly selected from the study cohort to derive predictors. Weighted odds ratios derived from logistic regression analysis were used to create a composite risk score and to stratify patients. The remaining 1/3 of the cohort (N=6,065) were used as the "validation cohort" to assess the accuracy value of the risk model.
Results:
A total of 18,194 patients who underwent IBR were identified from the ACS-NSQIP 2005-2011 database. The majority of patients were Caucasian (76.1%) and 45-64 years of age (62.4%). The average BMI was 27.1 ± 6.3 kg/m2. Bilateral reconstructions were performed in 38.6% of patients and the vast majority were inpatient (80.5%) and implant-based (80.2%). Overall, the study cohort was healthy with 57.5% of patients having no defined co-morbid conditions and an ASA score of 2 in 70.7%. Diabetes was present in 4.7% of patients; a total of 13.0% of the study cohort were active smokers. The most common co-morbid condition was hypertension
(23.6%). The average length of stay was 2.2 ± 4.1 days and the incidence of surgical complications was 7.2%.
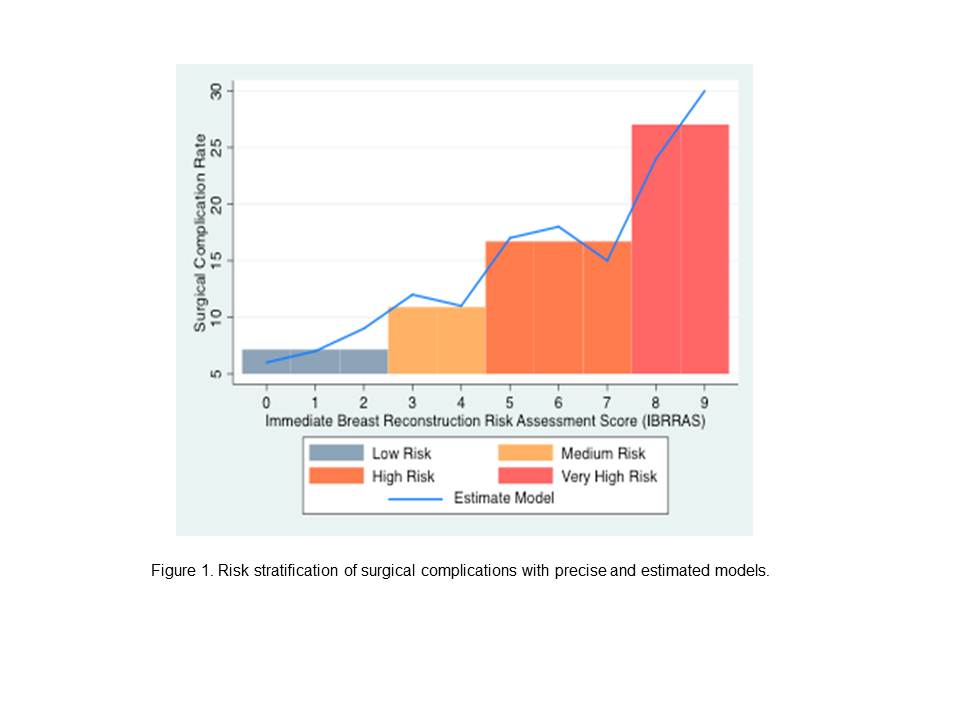
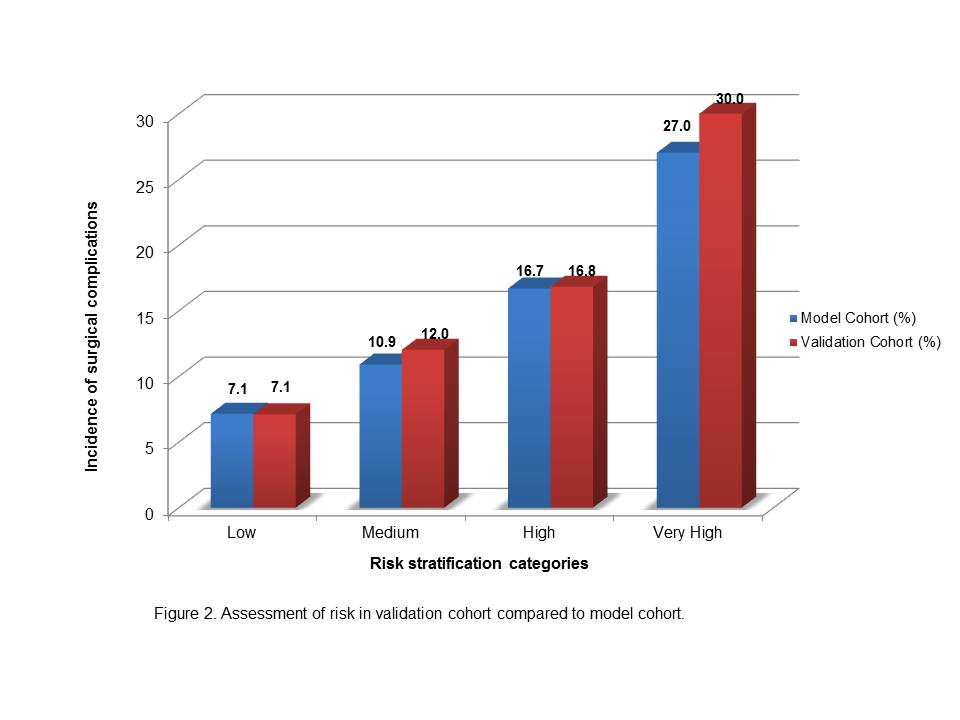
On adjusted analysis, autologous reconstruction (OR=1.41, P<0.001), ASA ≥3 (OR=1.25, P=0.004), obesity (OR=1.38, P<0.001), severe obesity (OR=1.91, P<0.001), morbid obesity (OR=1.70, P<0.001), and active smoking (OR=1.46, P<0.001) were associated with complications. Risk factors were weighted and patients were stratified into low (0 to 2, N=9,133, Risk=7.14%), intermediate (3 to 4, N=1,935, Risk=10.90%), high (5 to 7, N=1,024, Risk=16.70%), and very high (8 to 9, N=37, Risk=27.02%) risk categories based upon their total risk score (P<0.001) (Figure 1). Internal validation of the "model cohort" using the "validation cohort" was performed demonstrating accurate prediction of risk across groups: low (7.1% vs. 7.1%, P=0.9), intermediate (10.9% vs. 12.0%, P=0.38), high (16.7% vs. 16.8%, P=0.95), and very high (27.0% vs. 30.0%, P=1.0) (Figure 2).
Discussion:
Surgical complications following IBR are related to preoperatively identifiable factors which can be used to accurately risk stratify patients which may assist with counseling, selection, and perioperative decision-making. These factors can be used to risk stratify patients and may help in counseling, patient selection, and perioperative decision-making regarding modality and timing.
Back to Annual Meeting
|






