|
|
 |
Back to Program Outline
Back to Posters
Topic:
A Prospective Randomized Trial Comparing Subatmospheric Wound Therapy with a Sealed Gauze Dressing and the Standard Vacuum Assisted Closure Device: A Supplementary Sub-Group Analysis of Infected Wounds
Laurel S. Karian, MD1, Amir H. Dorafshar, MBChB2, Mieczyslawa Franczyk, PT, PhD2, Chad Teven, MD2, Kristen Wroblewski, MS2, Lawrence J. Gottlieb, MD, FACS2, Robert Lohman, MD, MBA,FACS3.
1University of Medicine and Dentistry of New Jersey, Newark, NJ, USA, 2University of Chicago, Chicago, IL, USA, 3Cleveland Clinic, Cleveland, OH, USA.
BACKGROUND:
Subatmospheric pressure wound therapy (SAWT) is commonly used to manage colonized and infected wounds. However, this practice remains controversial because the safety and efficacy of the technique has not been carefully documented. The patients described in this report are part of a prospective, randomized trial used to compare the effectiveness of two types of SAWT in hospitalized patients with acute wounds: Vacuum Assisted Closure (VAC) versus wall suction applied to a sealed gauze dressing (GSUC). The initial analysis showed that GSUC was not inferior to VAC with respect to changes in wound volume and surface area, but was less costly and less painful than VAC.
METHODS:
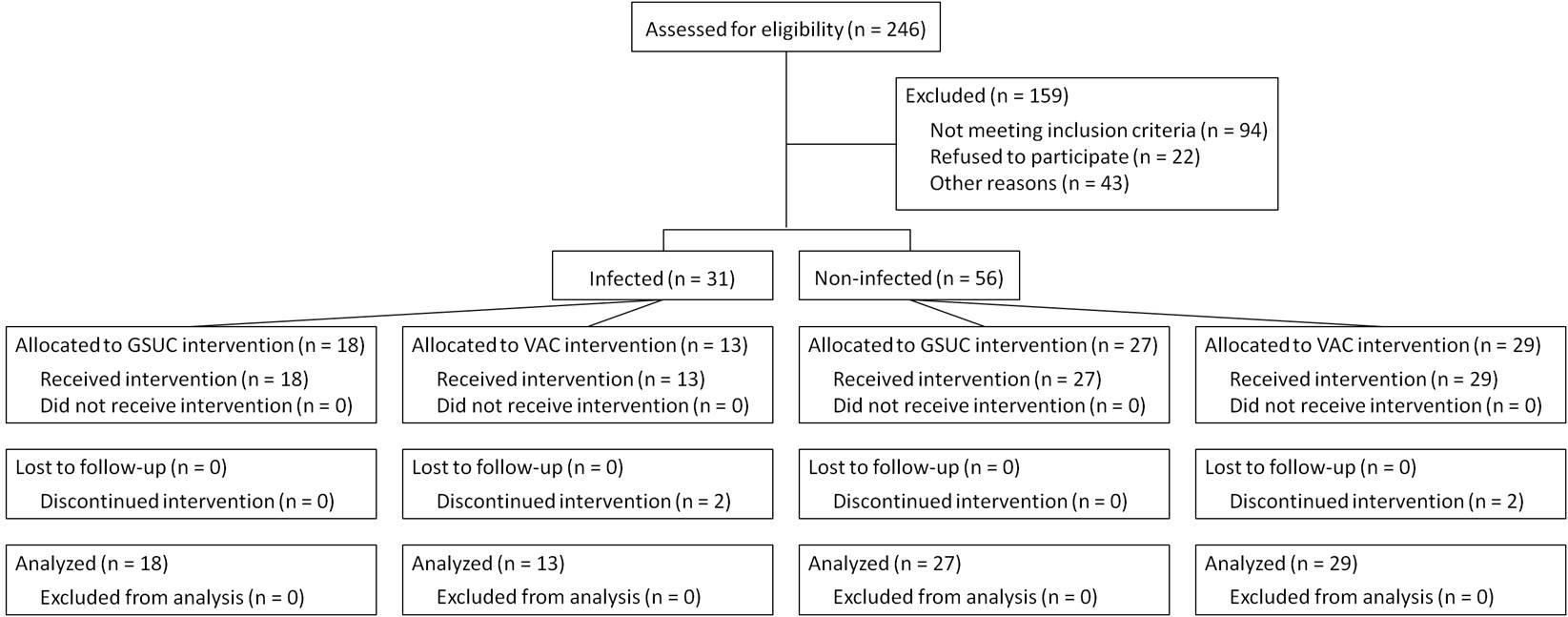
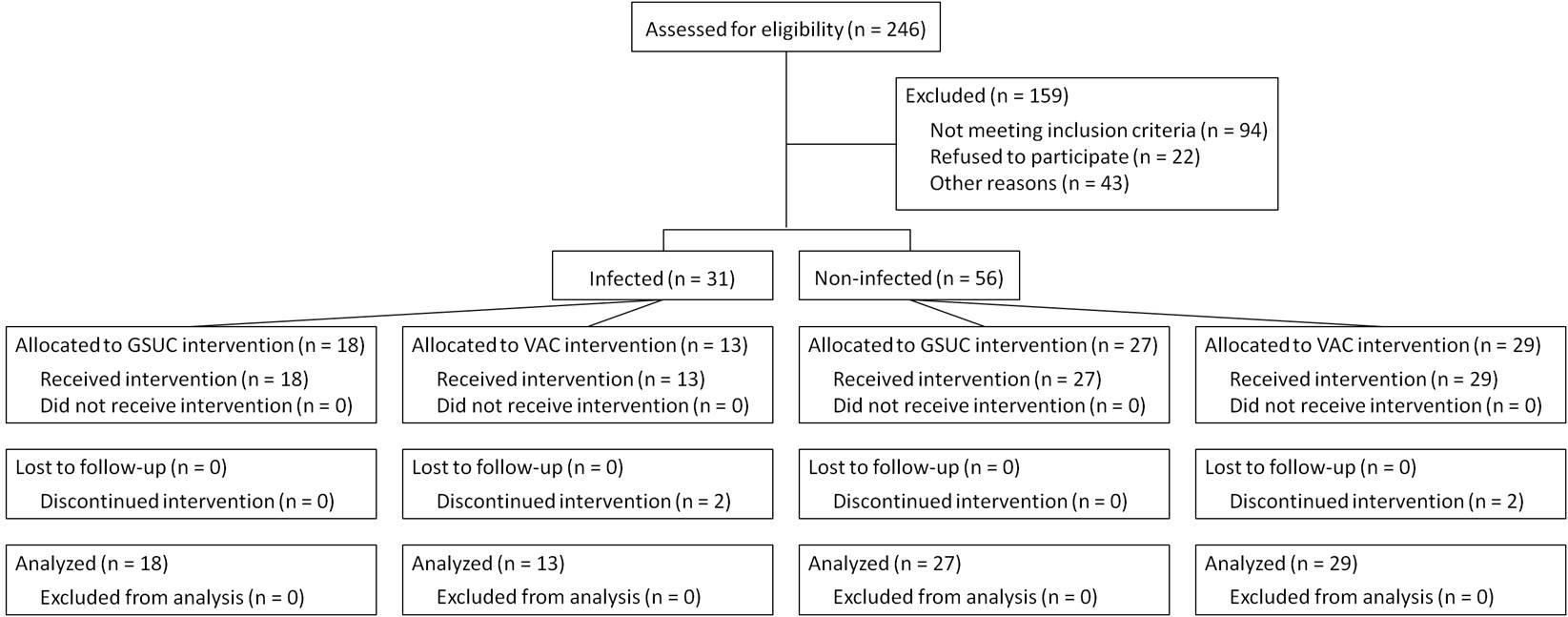
We assessed the safety and efficacy of GSUC compared to VAC in a subgroup of 31 patients with acutely infected wounds compared with 56 patients with non-infected wounds. Participants were 18 years or older who were admitted with acute wounds resulting from trauma, dehiscence or surgery, between October 2006 and May 2008. Exclusion criteria included wound malignancy, untreated osteomyelitis, allergy to sulfamylon and Dakin’s solution, and severe peripheral vascular disease. Patients with grossly necrotic wounds or systemic sepsis caused by wound infection were initially excluded, but were considered eligible after the wound was adequately debrided and sepsis had resolved. Wound infection was defined as the presence of an abscess with purulent material and a gram stain with > 105 colony forming units per gram of tissue. Both dressings were soaked with a topical antimicrobial solution three times a day while suction was on hold. Outcomes used to assess safety included development of wound necrosis, systemic sepsis, or other clinical complication. Outcomes used to assess efficacy were changes in wound surface area and volume, which were measured at each dressing change.
RESULTS:
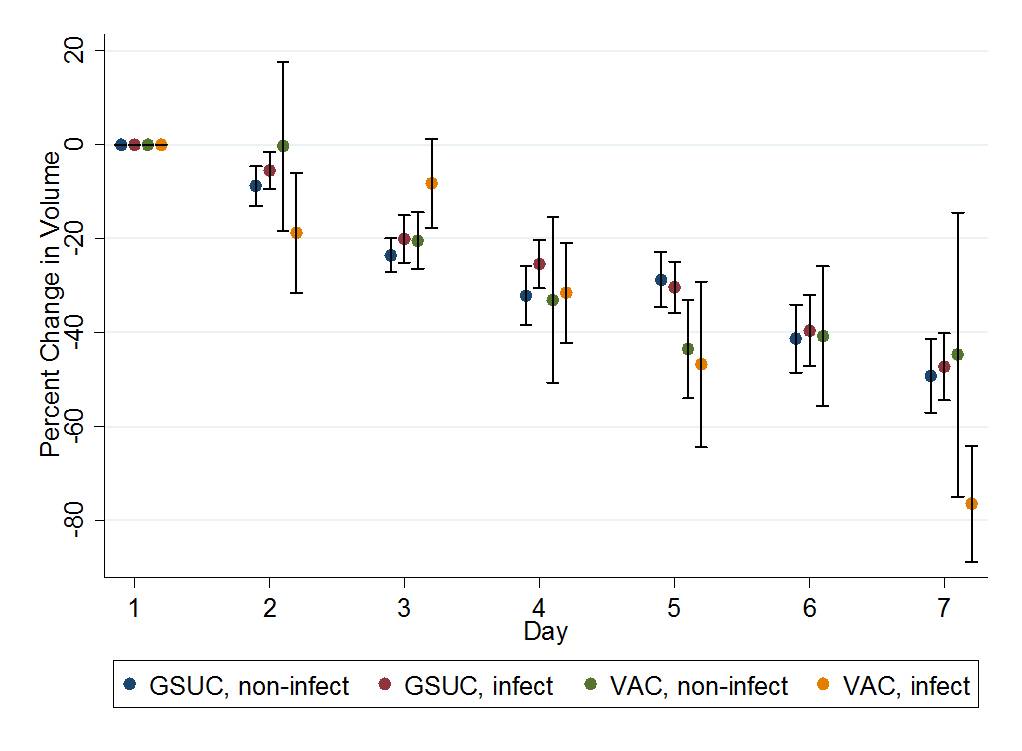
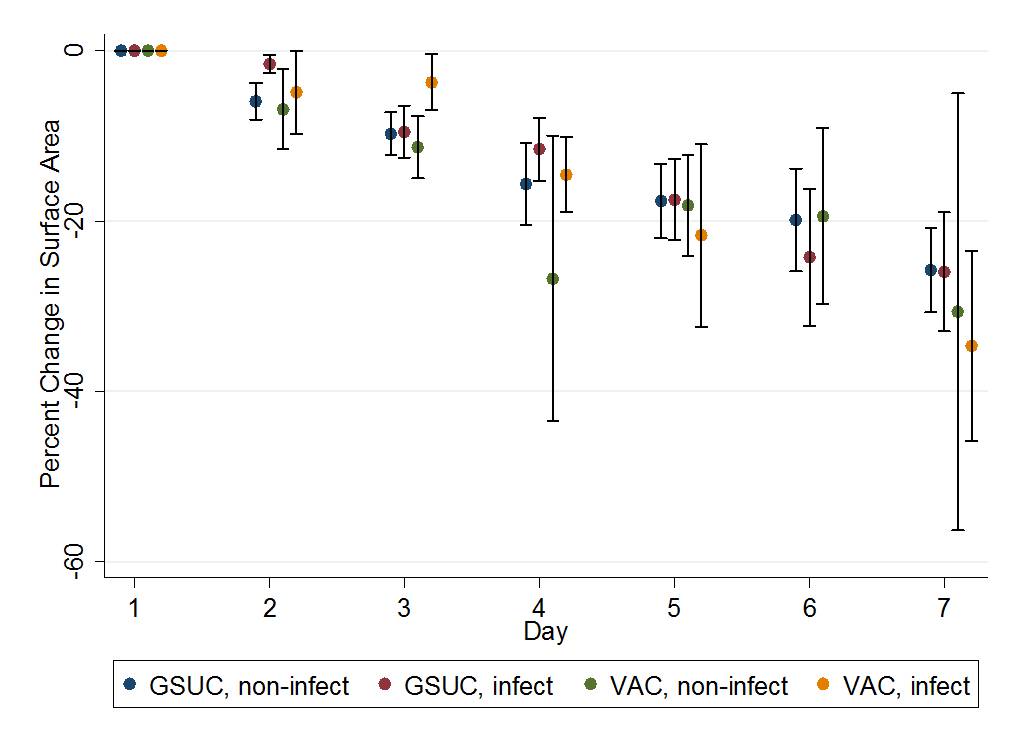
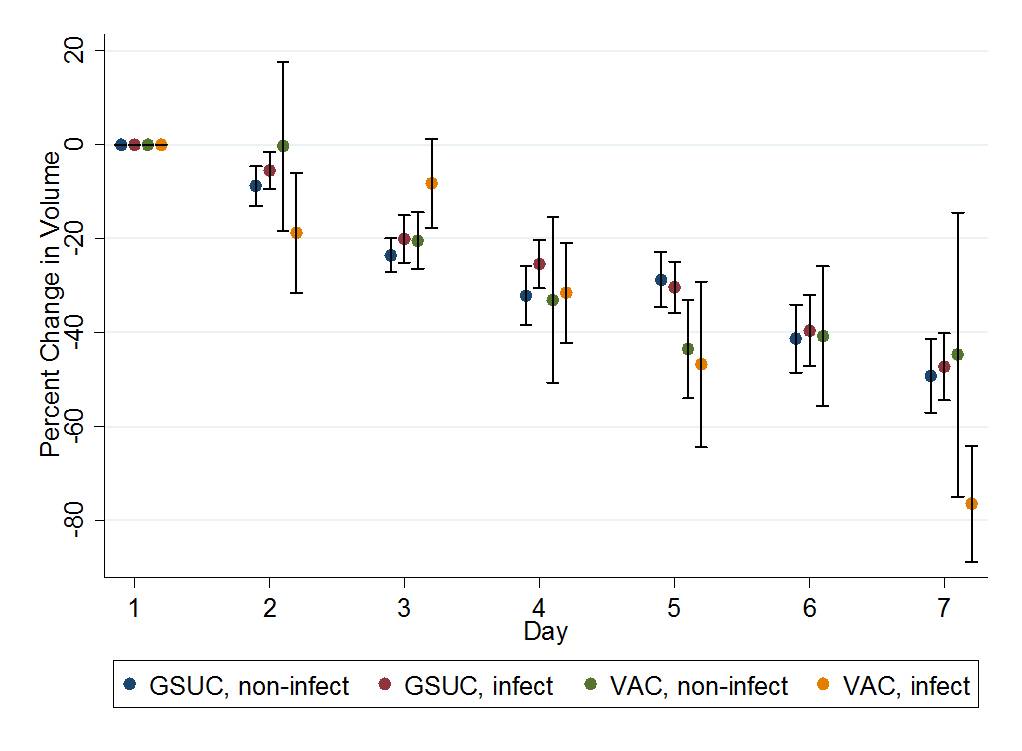
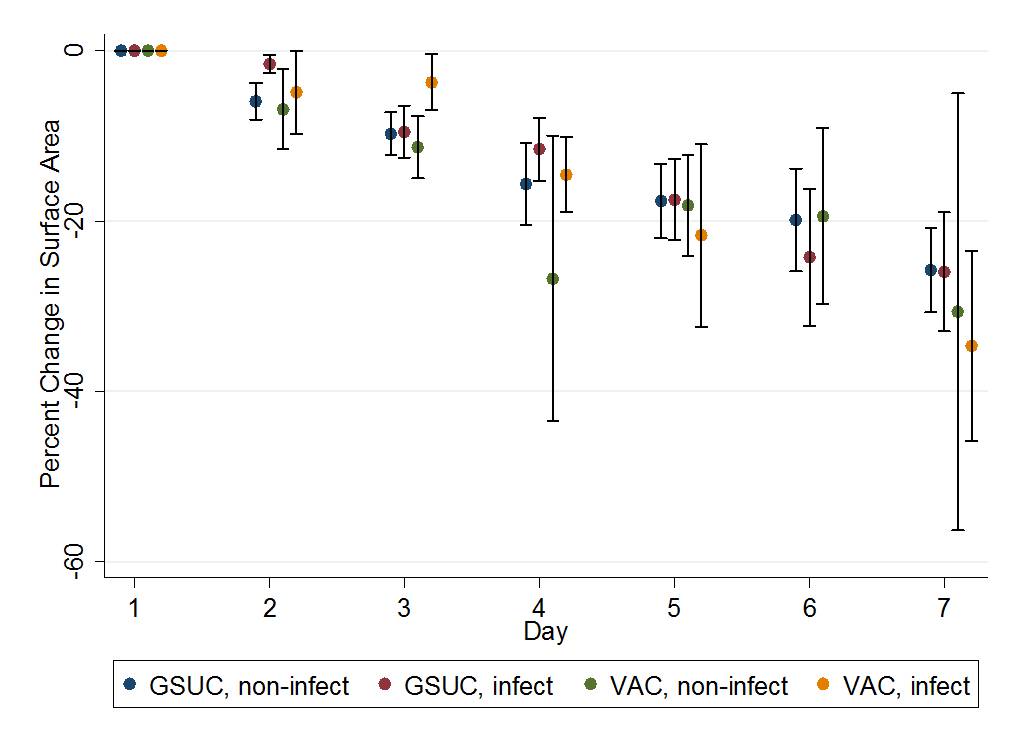
There were significant reductions in wound surface area and volume in both infected and non-infected groups; there was no significant difference in the rate of change observed in the GSUC versus VAC arms of the study. In the infected group, the reductions in wound surface area were 4.4%/day for GSUC and 4.8%/day for VAC, and in wound volume were 7.8%/day for GSUC and 9.7%/day for VAC (p<0.001 for all). Evidence of wound infection resolved in both groups by 96 hours, and there were no complications specifically related to the use of a sealed dressing over infected wounds.
CONCLUSIONS:
GSUC and VAC therapy can be used in selected acute, infected wounds and the two methods of treatment are similarly effective for reducing wound surface area and volume.
Back to Program Outline
Back to Posters
|