|
|
|
|
|
Back to 2014 Annual Meeting Abstracts
A Cost-utility Assessment of Mesh Selection in Clean and Clean-Contaminated Ventral Hernia Repair (VHR)
John P. Fischer1, Naveen M. Krishnan, MD2, Marten N. Basta, BA1, Jason D. Wink, MD1, Joseph M. Serletti, MD1, Stephen J. Kovach, III, MD1.
1University of Pennsylvania, Philadelphia, PA, USA, 2Georgetown University, Washington, DC, USA.
Introduction:
Ventral hernia is a common, challenging, and costly problem in the United States. Mesh-reinforcement can reduce recurrence, but selection is poorly understood, particularly in higher risk wounds. The use of acellular dermal matrixes (ADM) has provided a tool to perform single-stage ventral hernia repairs (VHR) in challenging wounds, but can be associated with higher complications, cost, and poor longevity. Cost-effectiveness techniques represent a useful analytic tool for better understanding the value of surgical interventions. The aim of this study is to perform a cost-utility analysis of ADM and synthetic mesh in clean and clean-contaminated (CC) VHR.
Methods:
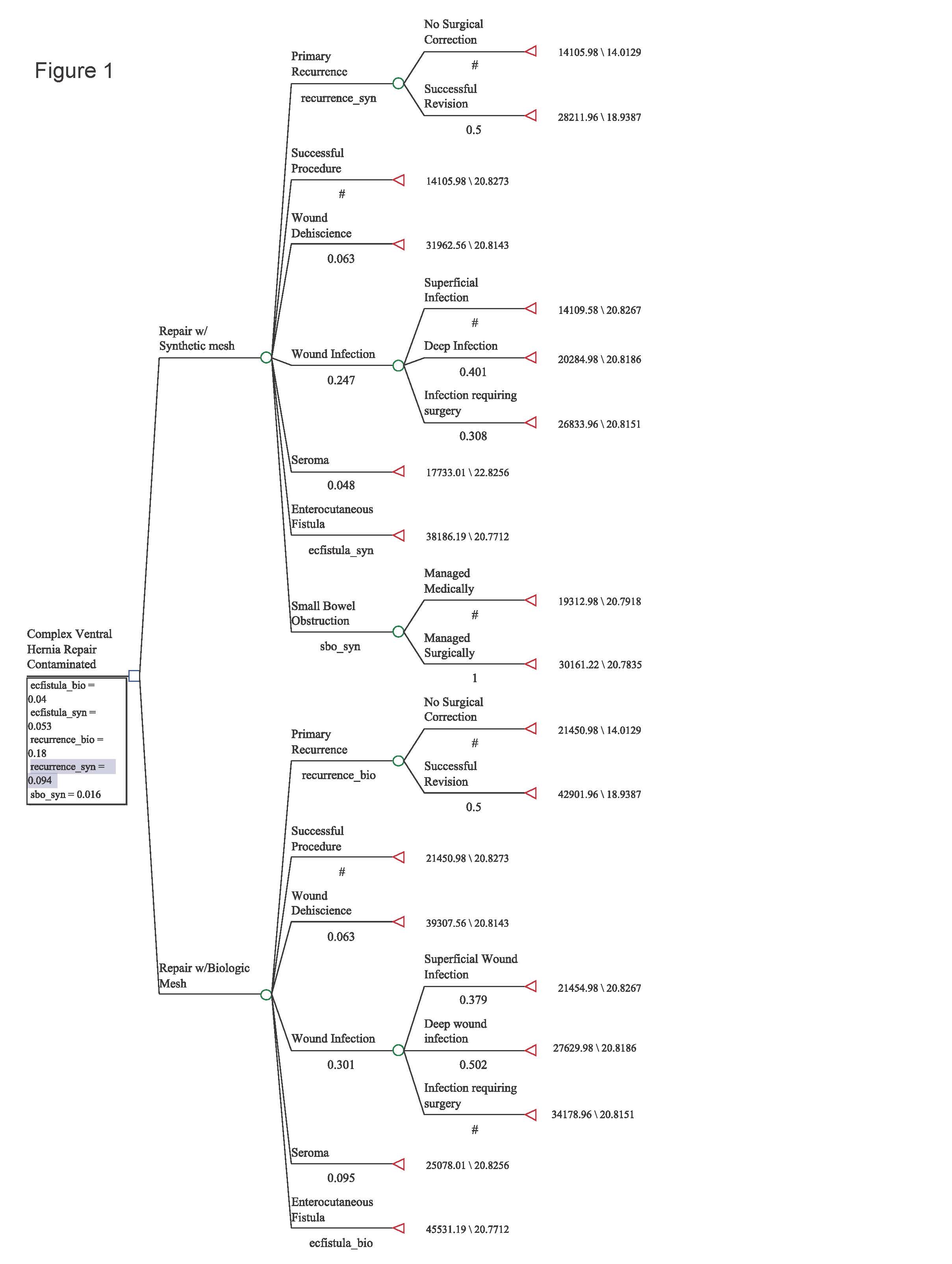
A systematic review was performed identifying articles containing comparative outcomes for synthetic mesh and ADM repairs. A web-based visual analog scale survey was administered to 300 nationally-representative community members to determine quality-adjusted life-years (QALYs) for several health states related to hernia repair (GfK Research). A Decision tree was created for the reference cases (VHR with ADM or synthetic) and up to six additional post-operative scenarios (Figure 1). Inputs included cost (DRG, CPT, and retail costs for mesh), quality of life, and health-outcome probability estimates. Overall expected cost and QALYs for VHR were calculated and compared using the roll-back method. The cost effectiveness threshold was set at $50,000/year-of-life gained (incremental cost utility ratio (ICUR)).
Results:
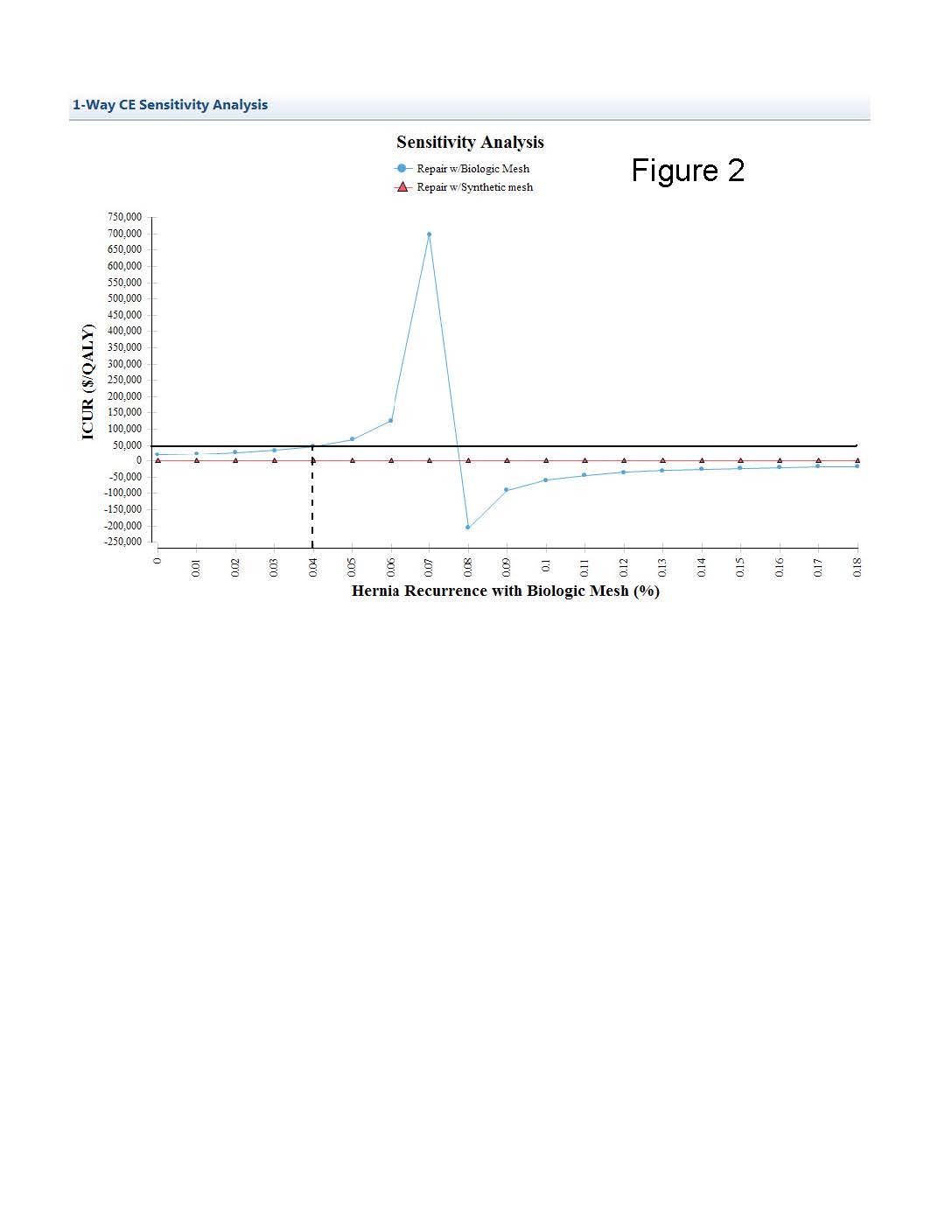
There was a 16% increase in the risk of a complication occurring after VHR when using biologic mesh compared to synthetic mesh in CC fields. This risk increased to 30% in clean fields. In CC fields, there was an increase of $8,022.61 in expected cost of VHR when using biologic mesh relative to synthetic mesh with a loss in clinical efficacy of 0.47 QALYs. This resulted in an ICUR of -$17,000/QALY (Figure 2). There was an expected increase of $11,694.02 with a clinical loss of 0.51 QALYs when using biologic mesh in clean fields resulting in an ICUR of -$23,000/QALY. Sensitivity analysis revealed that the recurrence rate of biologic mesh needs to be below 5% or the recurrence rate of synthetic mesh needs to be greater than 23% for biologic mesh to be cost effective in CC fields. In clean cases, the recurrence rate of synthetic mesh needs to be greater than 21% in order for biologic mesh to be cost effective.
Conclusions:
This cost-effectiveness analysis of mesh selection indicates that biologic meshes are not cost effective relative to synthetic mesh in clean or CC defects. Specifically, from a societal perspective synthetic mesh is both cheaper and more clinically effective than biologic mesh. Given the high prevalence of hernia and its associated cost to society, our data is critically important in improving cost-effective repair techniques, providing value-based care, and conserving healthcare resources in an ever-changing healthcare environment.
Back to 2014 Annual Meeting Abstracts
|
|




