Back to 2014 Annual Meeting Abstracts
Unplanned Hospital Readmission Following Body Contouring Procedures: An Analysis of 9,611 Patients From the National Surgical Quality Improvement (NSQIP) Databases
Ari M. Wes, BA, John P. Fischer, MD, Joseph M. Serletti, MD, Stephen J. Kovach, MD, Liza C. Wu, MD.
Hospital of the University of Pennsylvania, Philadelphia, PA, USA.
Purpose: To examine the incidence and predictors of 30-day unplanned hospital readmission following body contouring procedures.
Methods: We reviewed the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database from 2011 to 2012 for all body contouring cases. Bootstrap and multivariable logistic regression analyses (MVR) were employed to identify predictors of 30-day unplanned hospital readmission. Odds ratios from the MVR were used to define risk scores for each readmission predictor that reached statistical significance, these were summed to obtain the total readmission risk score for each patient.
Results: 9,611 patients underwent body contouring during the study period. Average BMI of patients undergoing body contouring was 31.0 kg/m2, while 1,013 individuals (10.6%) were morbidly obese (BMI 40 kg/m2). The most common areas of intervention were the breast and abdominal regions (N=6,752, 70.3%; N=2,556, 26.6% respectively). 8,584 (89.3%) patients underwent an isolated contouring procedure, while 906 (9.4%) underwent 2 procedures, and 121 (1.3%) underwent 3 or more.
Unplanned hospital readmission occurred in 375 (3.9%) individuals. Multivariate logistic regression revealed that ASA Class (Class>2: OR 1.64), undergoing abdominal contouring (OR 2.08), obesity (30≤BMI<35: OR 1.39; 35≤BMI7). The low risk cohort exhibited a readmission incidence of 1.6%, while the medium risk cohort experienced an incidence of 6.4%, and the high risk group an incidence of 19.3% (Figure 1). Importantly, 38 patients who required readmission (0.38% of the entire cohort; 10.1% of those requiring readmission) experienced major in-patient complications prior to the initial discharge (Figure 2); this group may represent a subset of readmissions that is exceptionally preventable and warrants further discussion.
Conclusion: These findings show that in the presence of certain risk factors, the incidence of hospital readmission increases dramatically; in these cases transitional care or other practices aimed at reducing unplanned readmission my be warranted.
Figure 1. Risk Scoring Model
Table 1. Risk factor weights. | | | Risk Factor | Risk Points | | 30≤BMI<35 | 1 | | 35≤BMI<40 | 2 | | BMI 40 | 3 | | Diabetes Mellitus | 2 | | History of COPD | 2 | | Smoking | 1 | | ASA Class > 2 | 1 | | In-patient | 3 | | Trunk Contouring | 2 | | >2 Distinct Regions Contoured | 1 |
Figure 2. Distribution of readmissions, outpatient major complications, and inpatient major complications. 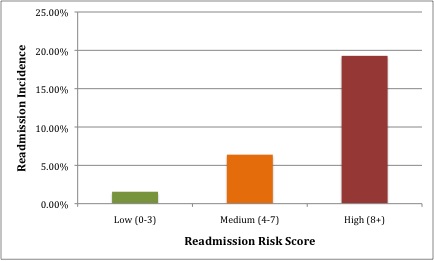 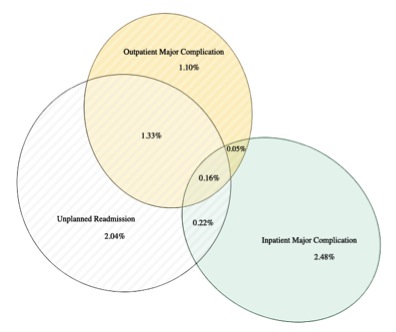
Back to 2014 Annual Meeting Abstracts
|




