|
|
|
|
|
Back to 2014 Annual Meeting Abstracts
A Propensity-Matched Analysis of the Influence of Breast Reconstruction on Subsequent Development of Lymphedema
Marten N. Basta, BA, John P. Fischer, MD, Joshua Fosnot, MD, Liza C. Wu, MD, Joseph M. Serletti, MD, Julia C. Tchou, MD, Yun R. Li, BS, Suhail K. Kanchwala, MD.
University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, USA.
Background
Lymphedema is a well-established complication of operative breast cancer treatment, particularly after axillary lymphadenectomy. Lymphedema predisposes patients to infectious complications, is physically debilitating, and significantly diminishes quality of life. Recent literature demonstrates breast reconstruction is associated with both a lower incidence of lymphedema and prolonged time to development of lymphedema. However, due to significant limitations in prior studies, the influence of reconstruction remains highly debated. This study aims to compare the incidence of lymphedema after axillary dissection in a propensity-matched cohort of patients with and without immediate breast reconstruction.
Methods
A retrospective review of all patients surgically treated for breast cancer from 1/1/2000-6/1/2013 was conducted. Only patients undergoing axillary lymphadenectomy with or without immediate breast reconstruction were included. Baseline demographics, including age, BMI (kg/m2), comorbidities, and neoadjuvant/adjuvant chemotherapy or radiation were collected. Operative characteristics noted were mastectomy laterality, reconstructive modality, ASA class, pathologic stage, and number of axillary nodes removed. The primary outcome, post-operative lymphedema, was defined by ICD-9 diagnosis. Univariate analysis of all demographic and operative characteristics was performed to identify baseline differences in patients undergoing reconstruction versus those who did not. Subsequently, each cohort was propensity-matched on the basis of age, obesity (BMI > 30 kg/m2), unilateral/bilateral mastectomy, cardiovascular disease, and hypertension. Among the matched cohorts, risk factors significantly associated with lymphedema in bivariate analysis were entered into a multivariate regression to identify independent predictors of lymphedema.
Results
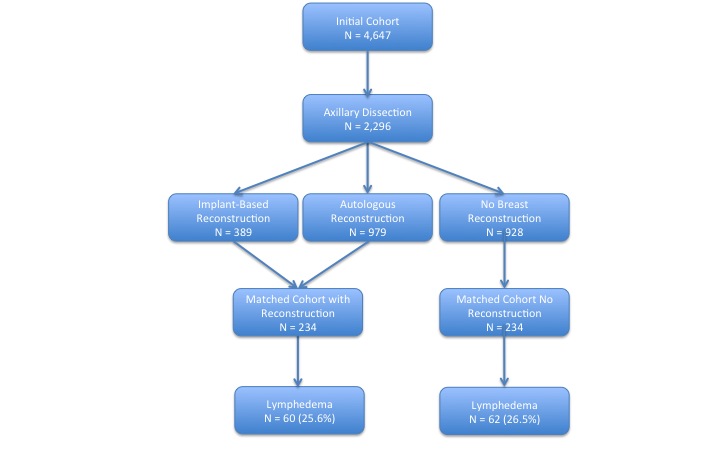
4,647 patients diagnosed with breast cancer were identified; axillary lymphadenectomy was performed in 2,296 patients who were included. Overall, 928 patients had no breast reconstruction, 979 had immediate autologous reconstruction, and 389 immediate implant-based reconstruction. Propensity-score matching yielded 234 patients without breast reconstruction and 234 undergoing breast reconstruction. Among the matched cohorts, only chronic kidney disease (p=0.03) and pulmonary comorbidity (p=0.02) remained more common in patients without reconstruction.
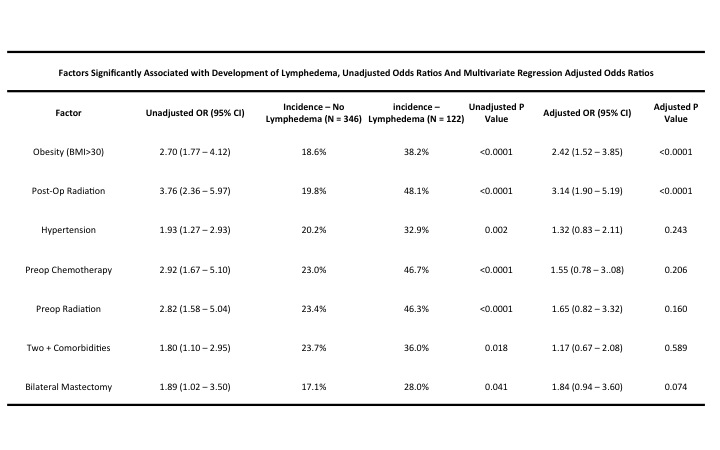
The incidence of lymphedema in the matched cohorts was 26.1% overall, and average time to diagnosis was 27.7 +/- 23.6 months postoperatively. Bivariate analysis found obesity, hypertension, bilateral mastectomy, presence of two or more comorbidities, history of chemotherapy, history of radiation, and post-operative radiation significantly increased risk of lymphedema(Table 1). Multivariate regression demonstrated that only obesity (OR=2.42, p<0.0001) and post-operative radiation (OR=3.14, p<0.0001) were independently predictive of lymphedema, although bilateral mastectomy approached significance (OR=1.84, p=0.074). Breast reconstruction was associated with a slightly lower incidence of lymphedema (OR=0.95, p=0.83).
Conclusions
We demonstrate the overall incidence of lymphedema after axillary dissection of 26.1%. Propensity-matched comparison showed that breast reconstruction, regardless of modality, does not significantly alter the development of lymphedema, while post-operative radiation and obesity greatly increase lymphedema risk. These evidence-based findings may enhance pre-operative guidance and better inform patient selection in an effort to mitigate severe complications.
Back to 2014 Annual Meeting Abstracts
|
|




