|
|
|
|
|
Back to 2014 Annual Meeting Abstracts
Functional Donor Site Morbidity Following Vascularized Toe Transfer Procedures: A Review of the Literature and Biomechanical Considerations for Surgical Site Selection
Michael Sosin, MD1, Yu-Te Lin, M.D.2, John Steinberg, D.P.M.3, Noah Oliver, D.P.M.3, Ketan M. Patel, M.D.2.
1R Adams Cowley Shock Trauma Center, Baltimore, MD, USA, 2Chang Gung Memorial Hospital, Taoyuan, Taiwan, 3MedStar Georgetown University Hospital, Washington, DC, USA.
Background:
Functional hand restoration and associated techniques are widely used and have been adopted into practice throughout the world. Despite these proven beneficial outcomes, less attention has been focused on donor site morbidity following such complex procedures. Specifically, the impact of toe harvest techniques as related to foot functionality may be overshadowed by the improvements in hand function. The purpose of this study was to conduct a systematic review and pooled analysis of vascularized toe-to-hand transfer to determine functional donor site morbidity among different techniques.
Methods:
A systematic literature search of Pubmed MEDLINE, EMBASE, and Cochrane databases was conducted in August 2013 to identify studies relating to toe-to-hand transfers and donor site morbidity in humans published between 1947 and 2013 yielding 302 citations, with 64 meeting inclusion criteria. Upon formal article review, data collection included: type of toe transfer, technique employed, etiology of digit injury, digit injured, level of injury, number of patients, gender, age, number of digits transferred per study, time of data collection, follow-up time, donor site assessment tools, and donor site findings. Assessment of donor site morbidity was divided into subjective and objective assessment. Pooled outcomes and analysis is reported.
Results:
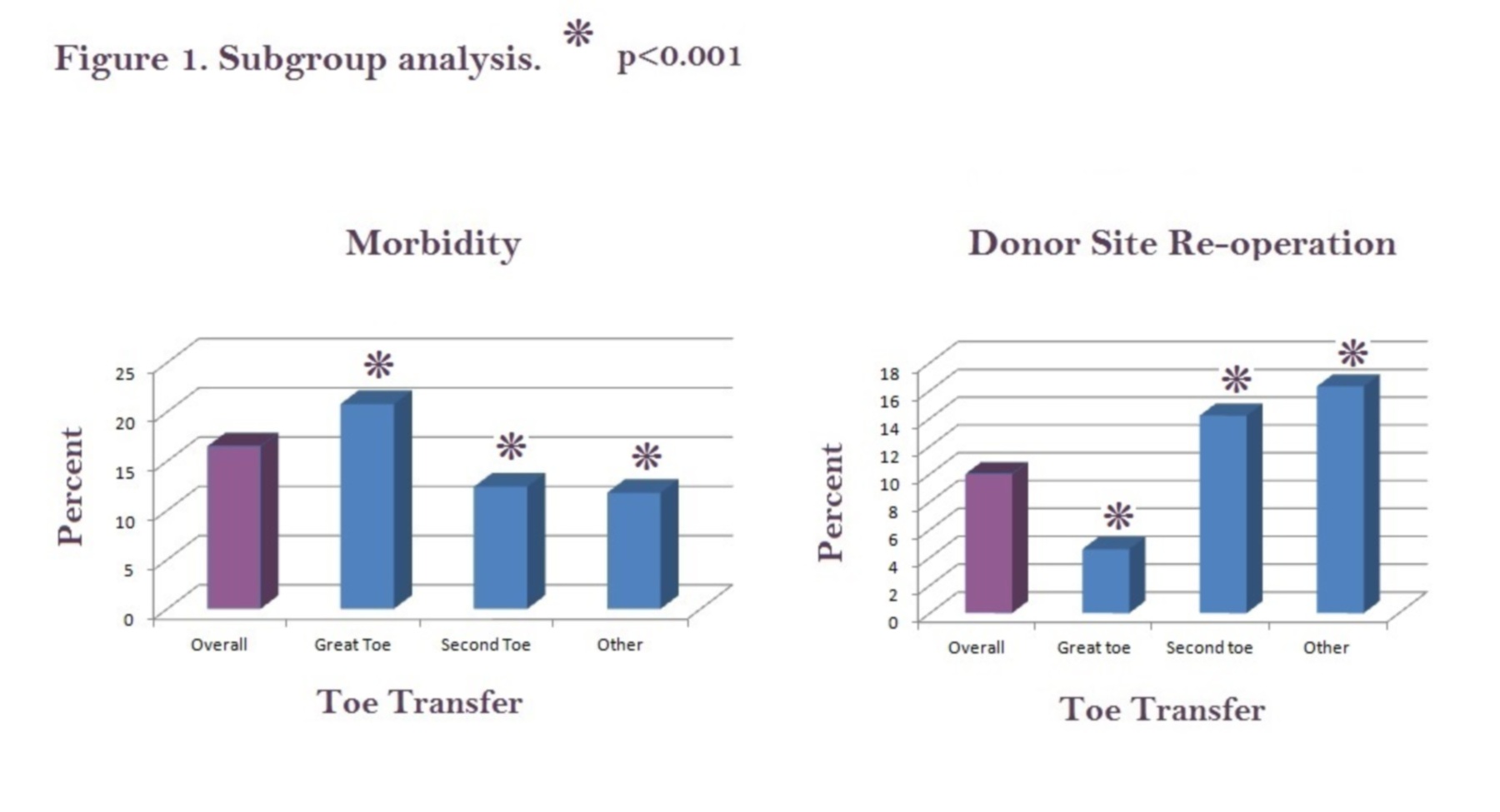
A total of 954 digits transfers (442 isolated great toe transfers, 379 isolated second toe transfers, and 153 transferred toes classified as ‘other’) were analyzed (80.8% male, 19.2% female). Etiology of injury was traumatic in greater than 99% of cases. Overall functional impairment analysis found 23.7% (97 digit transfers) experienced gait impairment, while 76.3% (313 digit transfers) reported no functional impairment. Subgroup analysis is depicted in Figure 1. 27.8% of free great toe transfers manifested some form of gait impairment versus 19.9% of great toe wraparound transfers. Five studies demonstrated imbalance of force in improper anatomical distribution, with two studies showing increased load on the 4th/5th metatarsal heads, and piezoelectric gait analysis showing impaired propulsion during gait. Preserving the ray resulted in hallux rigidus at the MTP resulting in increased load over the 3rd/4th metatarsal heads, valguization of the second toe with radiographic misalignment, and impairment in the pushoff phase of gait. However, 3 other forms of dynamic pedobarography, and 10 subjective reports from patients and physicians found no or less impairment in gait. Mean follow-up time was 62.6 months.
Conclusions:
Functional foot impairment can occur following various toe transfer procedures due to altered biomechanics of weight distribution and gait. Rigorous biomechanical foot evaluation of this subset of patients is lacking, but current data suggests certain distinct findings. Great toe transfer appears to have the highest morbidity rate, but lower re-operative intervention as compared to second toe transfer. Preserving ray projection does not prevent biomechanical changes to the foot, but may delay functional impairment leading to favorable functional interpretation by patients and surgeons.
Back to 2014 Annual Meeting Abstracts
|
|




