|
|
|
|
|
Back to 2014 Annual Meeting Abstracts
Vascularized Bone vs. Fasciocutaneous Free Flaps for Mandibular Reconstruction: A Retrospective Comparison of Outcomes and Complications
Marten N. Basta, BA, Patrick A. Gerety, MD, Gregory Epps, BA, John P. Fischer, MD, Jonas Nelson, MD, Suhail K. Kanchwala, MD, David W. Low, MD, Liza C. Wu, MD.
University of Pennsylvania, Philadelphia, PA, USA.
Background
Mandibular reconstruction has been revolutionized by the use of free tissue transfer over the past three decades. While vascularized bone flaps have demonstrated reliability, there remains controversy about the algorithm for bony vs. soft tissue reconstruction. The aim of this study was to evaluate mandibular reconstruction with free tissue transfer comparing vascularized bone and vascularized soft tissue.
Methods
A retrospective institutional review was conducted identifying all patients undergoing free flap reconstruction of mandibular defects from 1/1/2005 - 6/1/2013. Patient characteristics, including age, BMI, medical comorbidity, indication for reconstruction, as well as history of chemotherapy or radiation therapy were recorded. Defect characteristics were described by location, extent, as well as laterality. Flap type, use of titanium plating, and flap modifications were included as operative characteristics. The primary outcome of interest was major surgical complication, defined as flap thrombosis, any flap loss requiring intervention, and wound complication requiring reoperation. Secondary outcomes included average post-operative interval to oral diet and interval to tracheostomy decannulation. Univariate analysis of patient and operative factors identified significant associations with major surgical complications. Subsequent multivariate regression was performed to determine if there were any independent predictors of complications by flap selection.
Results
A total of 111 patients undergoing free flap reconstruction of mandibular defects were included, 59 of whom had a fibula flap and 52 a soft-tissue flap. Comparison of baseline demographics demonstrated that patients having fibula flaps were generally younger (Age<45 years=22.0% vs. 4%, p=0005), with post-traumatic defects (9% vs. 0%, p=0.059), and underwent delayed reconstruction more commonly (14% vs. 2%, p=0.034). Patients reconstructed with soft tissue flaps had higher rates of cardiovascular disease (69% vs. 37%, p=0.001) and squamous cell carcinoma (89% vs. 43%, p<0.0001). Fibula reconstructions were typically larger defects (hemimandibulectomy=27% vs. 21%, p=0.034), involved anterior and central defects (42.3% vs 33.4%, p=0.065), and required titanium plating more (94.9% vs 40.4%, p<0.0001).
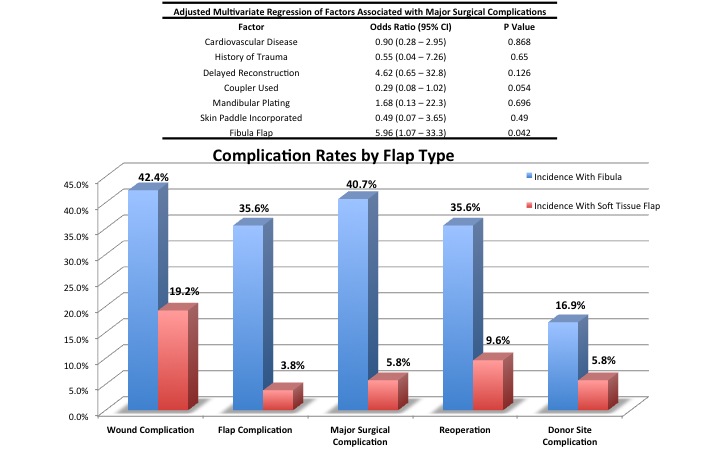
Major surgical complication rate was 41% for fibula flaps and 6% for soft tissue flaps (p<0.0001). Flap complications were also more common with bony reconstruction (36% vs 4%, p<0.0001). Patients with soft tissue flaps were more likely to be discharged with a PEG tube (61% vs. 48%, p=0.01) or a tracheostomy tube (94% vs. 77%, p=0.02); however, neither average time to oral diet nor time to decannulation differed by flap type. Multivariate regression demonstrated that only flap type was an independent risk factor for major surgical complications (OR=5.96, p=0.04).
Conclusions
This study demonstrates that soft tissue flaps are comparable to osteocutaneous flaps regarding efficacy and may have a favorable risk profile. While patient and defect characteristics inherently differ, multivariate regression demonstrated that fibula flaps were independently associated with worse outcomes. Flap selection remains a critical component of perioperative decision-making; soft tissue reconstruction appears to be an appropriate option in certain patients.
Back to 2014 Annual Meeting Abstracts
|
|




