|
|
|
|
|
Back to 2014 Annual Meeting Abstracts
A Perioperative Model for Medical and Surgical Complications in Complex Head and Neck Microvascular Reconstruction
Patrick A. Gerety, MD, Marten N. Basta, BA, John P. Fischer, MD, Megan Fracol, BA, Suhail K. Kanchwala, MD, Joseph M. Serletti, MD, David W. Low, MD, Liza C. Wu, MD.
University of Pennsylvania, Philadelphia, PA, USA.
Background
Free tissue transfer has become the standard of care for reconstructing head/neck defects. Medical and flap complications have been associated with tremendous hospital costs in these patients, and a better understanding of predisposing factors is essential to improve cost-efficacy and patient satisfaction. This project aims to create the first preoperative risk-stratification tool in head/neck reconstruction based upon our free flap experience.
Methods
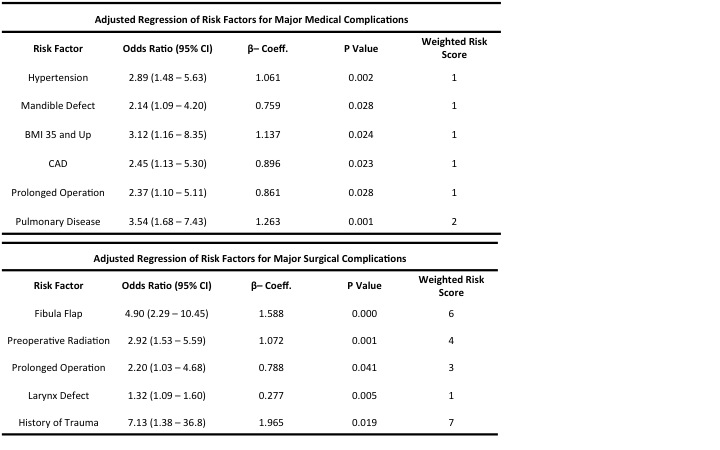
An institutional retrospective chart review identified all free flap head/neck reconstructions performed from 2005-2013. Demographic information and operative characteristics were collected as preoperative risk factors. Intra/post-operative complications and total hospital cost for were detailed. Primary outcomes were flap complication (anastomotic revision, arterial/venous flap thrombosis, or partial/full flap loss) and medical complication (heart failure, MI, acute renal failure, VTE, pneumonia, respiratory failure, septicemia, or stroke). Preoperative factors were analyzed via step-wise multivariate logistic regression, with significant variables entered into a bootstrap model. Final adjusted beta-coefficients were utilized to generate weighted risk scores for each variable. Each patient was assigned an aggregate risk score for each complication, yielding the risk-assessment tool.
Results
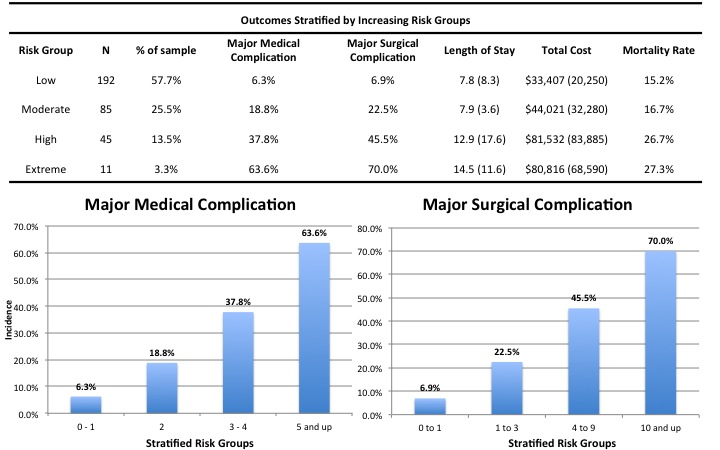
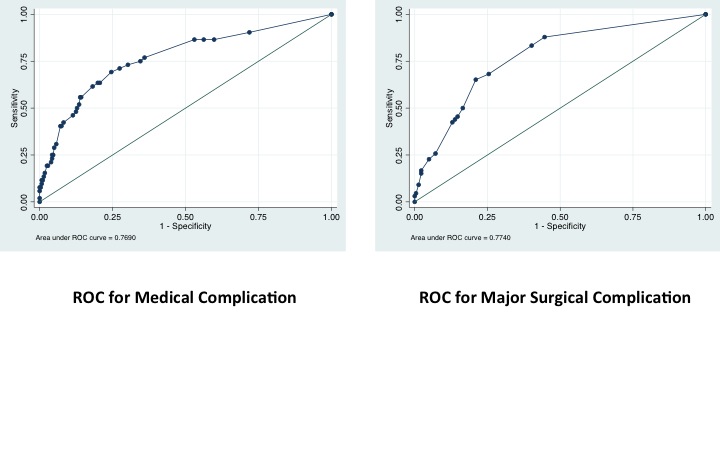
438 free flap head/neck reconstructions were included. Medical complication incidence=14.4% and significant predictors included BMI>35 (OR=3.12), coronary artery disease (OR=2.45), mandibular defect (OR=2.14), hypertension (OR=2.89), pulmonary disease (OR=3.54), and prolonged operative time (OR=2.37). Patients were risk-stratified into 4 groups: low (complication=6.3%), moderate (complication=18.8%), high (complication=37.8%), and extreme (complication=63.6%). Major surgical complications incidence=19.4%, with predictors including prolonged operative time (OR=2.20), radiation (OR=2.92), larynx defect (OR=1.32), history of trauma (OR=7.13), and fibula flap (OR=4.90). Patients were risk-stratified into 4 groups: low (complication=6.9%), moderate (complication=22.5%), high (complication=45.5%), and extreme (complication=70%). Patients at intermediate/high risk of medical or flap complications had significantly longer hospital stay, more reoperations, and higher mortality rate. Total hospital costs for patients at extreme-risk for medical complications were $80,816 vs. $33,407 for low-risk patients. The risk models demonstrated high accuracy for discriminating complication risks with C-statistic=0.77 (medical) and C-statistic=0.774 (major surgical).
Conclusion
This study identifies important independent preoperative risk factors for medical and major surgical complications in head/neck microsurgical reconstruction with high accuracy. Importantly, the model stratifies patients according to risk, demonstrating that higher risk groups suffer significantly more morbidity and incur substantially higher costs. As the first such model in head and neck microvascular reconstruction, it can serve as a simple yet accurate tool for perioperative decision-making.
Back to 2014 Annual Meeting Abstracts
|
|




