Back to 2014 Annual Meeting Abstracts
Obesity-Induced Lymphedema: Presentation, Diagnosis, and Management
Reid A. Maclellan, MD, MMSc, Frederick D. Grant, MD, Sumner A. Slavin, MD, Arin K. Greene, MD, MMSc.
Children's Hospital Boston / Harvard Medical School, Boston, MA, USA.
Background: Lymphedema results from inadequate transport of lymphatic fluid, and typically affects the extremities. The condition may be caused by maldevelopment of lymphatics (primary) or by injury to lymph nodes or vessels (secondary). Recently, obesity has been recognized as a novel cause of lower extremity lymphedema. The purpose of this study was to characterize patients with obesity-induced lymphedema.
Methods: Patients referred to our Lymphedema Program between 2009 and 2014 with possible lower extremity lymphedema were reviewed. Individuals with a body mass index (BMI) >30 who underwent lymphoscintigraphy to assess lymphatic function were studied. Patients with a history of primary lymphedema, lymphadenectomy, or nodal radiation were excluded. Gender, age, maximum BMI history, BMI at the time of lymphoscintigraphy, and location of lymphedema were recorded.
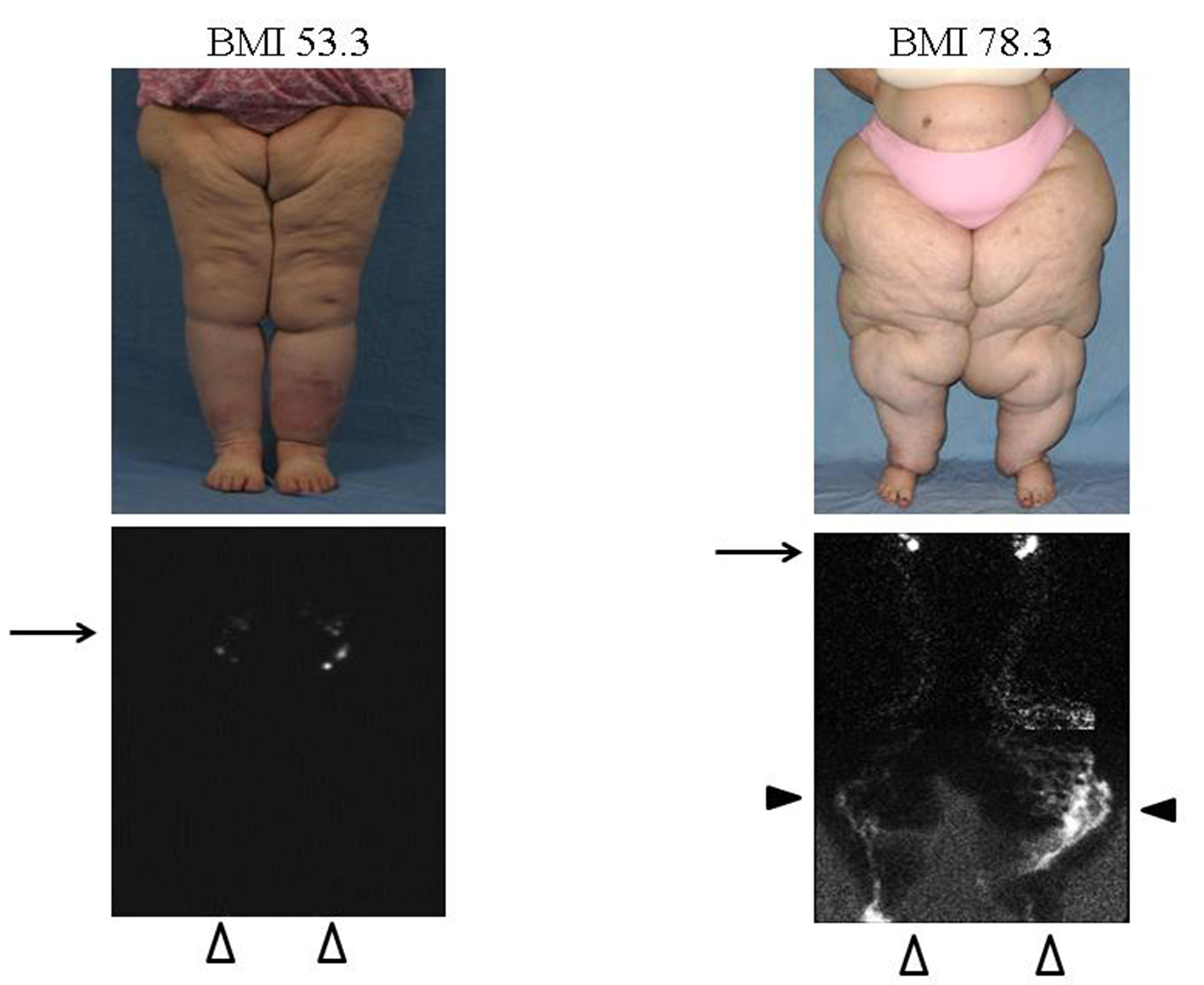
Results: Forty patients met inclusion criteria; mean age was 54.6 years (range 14-85 years). Lymphoscintigraphy showed that 27 patients had normal lymphatic function and 13 patients (7 females, 6 males) had lymphatic dysfunction consistent with obesity-induced lymphedema. Individuals with lower extremity lymphedema had a BMI at the time of the lymphoscintigram of 64.1 (range 43.9-83.0), and a maximum BMI history of 76.1 (range 60.5-105.6). Obese patients with normal lymphoscintigraphy findings had a BMI at the time of their study of 38.5 (range 30.3-56.8), and a maximum BMI history of 44.4 (range 30.3-85.4) (Figure 1). The patient with the highest BMI history of 105.6 also had bilateral upper extremity lymphedema confirmed by lymphoscintigraphy. One patient with obesity-induced lymphedema (BMI 80.1) had improved lymphatic function by lymphoscintigraphy after reducing her BMI to 70.9.
Conclusions: Massive obesity can cause extremity lymphatic dysfunction. A BMI threshold appears to exist at which point lower extremity lymphedema occurs, followed by upper extremity disease. Patients with obesity-induced lymphedema are referred to a bariatric center because weight loss appears to improve lymphatic function, but may not reverse the condition.
Figure 1: Obesity-induced lower extremity lymphedema; a BMI threshold appears to exist between 53-59 when lymphatic dysfunction occurs. (Left) Adult female with a BMI of 53.3. Lymphoscintigraphy illustrates normal transit to inguinal nodes 20 minutes following injection. (Right) Adult female with a BMI of 78.3. Lymphoscintigram shows delayed transit of tracer to inguinal nodes 3 hours following injection, tortuous
collateral lymphatic channels, and dermal backflow consistent with lymphedema. Arrows indicate inguinal nodes, black arrowheads show tortuous lymphatic channels and dermal backflow, and white arrowheads mark the feet where the radiolabelled tracer was injected.
Back to 2014 Annual Meeting Abstracts
|




