|
|
|
|
|
Back to 2014 Annual Meeting Abstracts
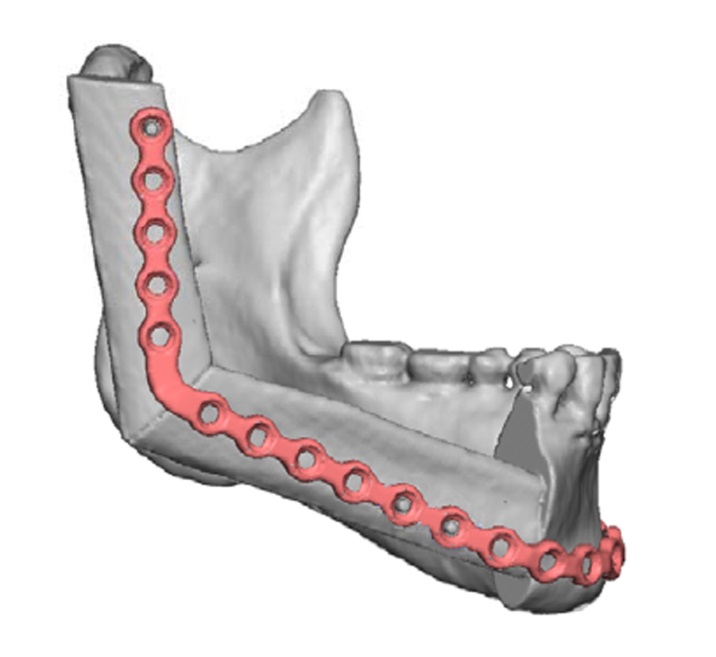
Keeping it simple: Improving dental outcomes with osseointegrated implants after “single barrel” free fibula reconstruction of the mandible
Jerry W. Chao, M.D.1, Christine H. Rohde, M.D.2, Michelle M. Chang, B.S.2, David I. Kutler, M.D.1, Joel Friedman, D.D.S.1, Jason A. Spector, M.D.1.
1Weill Cornell Medical Center, New York, NY, USA, 2Columbia University Medical Center, New York, NY, USA.
BACKGROUND:
The free fibula flap has become the workhorse for reconstruction of the mandible after resection for tumor or osteonecrosis, with aesthetics and dental rehabilitation being the primary goals of reconstruction. A shortcoming of the fibula flap is its lack of height compared to the native mandible. As a result, osseointegrated implants placed into the fibula may be vertically short of the native occlusal plane. Approaches to address the fibula’s height deficiency have included the “double-barrel” fibula and vertical distraction osteogenesis. However, these confer additional complexity and risk to the reconstruction. Others have placed onlay bone graft, though this requires further surgery and donor site morbidity and carries the risk of graft loss and infection. We hypothesized that mandible reconstruction using a single barrel fibula placed several millimeters above the inferior border of the native mandible would allow for improved dental rehabilitation without any untoward aesthetic consequences.
METHODS:
A retrospective chart review was performed for all patients undergoing free fibula reconstruction of the mandible at our institution since 2006. Patients included for study were those who underwent placement of osseointegrated implants or other secondary prosthodontic procedures. Charts were reviewed for use of computer-aided modeling, post-operative aesthetics, and tolerated diet. Panorex images were analyzed at standardized positions for fibula height, mandibular height, crown-to-implant (C/I) ratio, and vertical placement of the fibula.
RESULTS:
Nine patients were identified for study out of a total 44 mandibular reconstructions. Computer-aided modeling was used to plan reconstruction in all study patients, and fibula placement was determined preoperatively during the planning session in conjunction with ablative and oral surgeons. Six patients were reconstructed with the fibula placed above the inferior border of the mandible (group A), and three had the fibula aligned with the inferior border of the mandible (group B). Average follow-up was 18 months.
Implants in group A were placed into shorter fibulas (group A 14.4mm vs group B 16.0mm, p=0.04), and the average native mandibular height was greater in group A (37.7mm vs 32.1mm, p=0.002). The fibula was positioned an average of 4.7mm (range 4.3-6.0mm) above the inferior border of the mandible in group A, with improved C/I ratio and alignment of the final crown. Average C/I ratio in group A was 1.66±0.57, representing a decrease of 19.7% compared to if these fibulas had been aligned with the inferior mandibular border. All patients tolerated a regular diet post-operatively. All patients had good post-operative aesthetics and symmetry.
CONCLUSIONS:
The single-barrel fibula may be placed 4-5mm above the inferior border of the mandible to improve alignment of osseointegrated implants with the native occlusal plane without any detrimental effect on the aesthetic result. Computer aided modeling is useful for precisely planning fibula positioning for further prosthodontic reconstruction.
Back to 2014 Annual Meeting Abstracts
|
|




