|
|
|
|
|
Back to 2014 Annual Meeting Abstracts
PEMF Accelerates Reduction of Post-Operative Pain and Inflammation: Application to Plastic and Reconstructive Surgical Procedures
Christine H. Rohde, MD, MPH, FACS1, Erin M. Taylor, BA1, Jeffrey A. Ascherman, MD, FACS1, Krista L. Hardy, BS1, Arthur A. Pilla, PhD2.
1Columbia University Medical Center, New York, NY, USA, 2Departments of Biomedical Engineering, Columbia University and Orthopedics, Mount Sinai School of Medicine, New York, NY, USA.
BACKGROUND: Non-invasive pulsed electromagnetic field (PEMF) therapy is known to reduce pain and inflammation by enhancing nitric oxide (NO) signaling which, in turn, increases blood flow and modulates pro-and anti-inflammatory cytokines. This study reports the effect of PEMF, configured to modulate NO signaling, on post-operative pain, wound exudate volume, and IL-1β concentration (a pro-inflammatory cytokine involved in pain hypersensitivity) in breast reduction (BR) and transverse rectus abdominis myocutaneous flap breast reconstruction (TRAM flap) patients.
METHODS: An identical non-thermal pulsed radio frequency PEMF signal consisting of a 2 msec burst of a 27 MHz carrier repeating at 2 bursts/sec, and inducing 5 ± 1 V/m electric field, was applied immediately post-operatively to 24 BR and to both breast and abdominal sites for 32 TRAM flap patients in double-blind, placebo-controlled, randomized studies. All patients had Jackson-Pratt drains at all surgical sites. Pain scores by patient-assessed visual analog scale (VAS) and total exudate volumes were recorded at intervals starting at one hour post-operative. Exudates were stored at -80oC for subsequent IL-1β determinations using ELISA.
RESULTS: In each figure, results are summarized for BR (left image) and TRAM flap (right image) studies, respectively. VAS scores, summarized in Fig. 1, show that PEMF accelerated the initial rate of pain decrease by approximately 3-fold in active cohorts, with pain 3-fold higher at 48 hrs in sham cohorts (P < 0.01). Fig. 2 shows that cumulative wound exudate volume increase was nearly 2-fold higher in sham cohorts (P < 0.001). Fig. 3 shows that IL-1β in wound exudates increased nearly 3-fold faster over the first 5 hrs in sham cohorts, and that IL-1β is more than 3-fold higher in sham cohort exudates 6-24 hrs post-operative (P < 0.02).
CONCLUSIONS: This study shows that non-thermal PEMF therapy produces rapid reductions in post-operative pain and markers of inflammation for both simple and complex surgical procedures. These effects translate to decreased post-operative narcotic use and morbidity during recovery, as reported elsewhere. Although the mechanism of action of PEMF in these studies is not yet completely elucidated, the effects reported here are consistent with a mechanism based upon an effect on NO signaling. PEMF therapy has no known adverse effects and is a simple, non-pharmacological adjunct for the management of post-operative pain and inflammation, which could enhance surgical recovery.
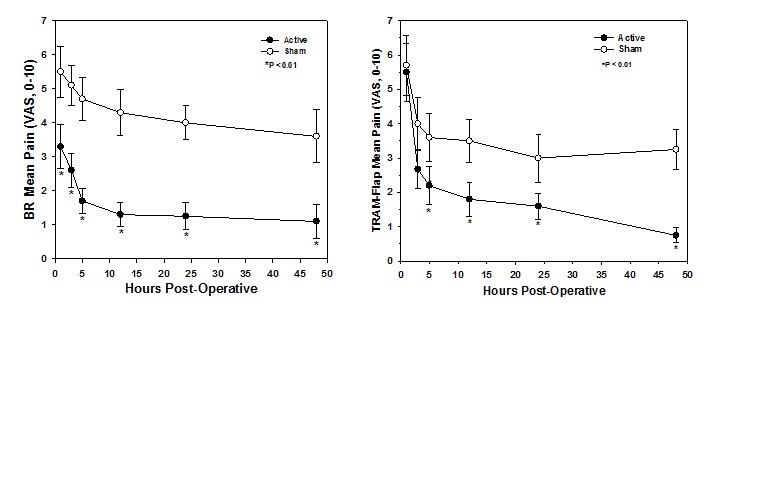
Fig 1: Effect of PEMF Therapy on post-op pain reduction.
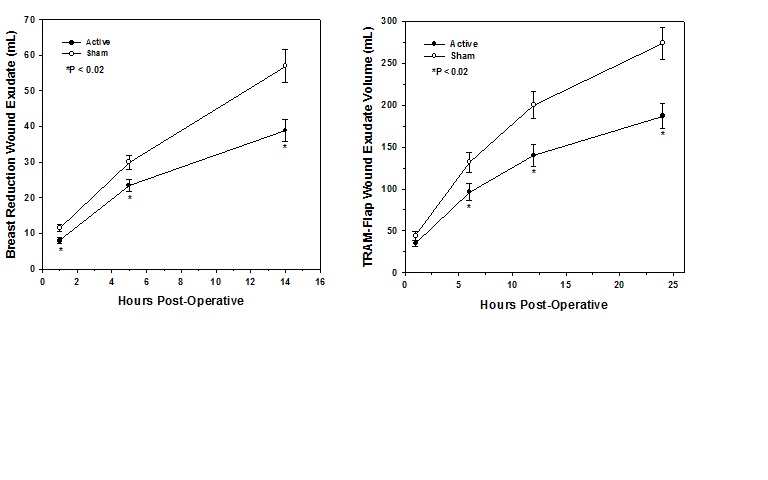
Fig 2: Effect of PEMF on cumulative wound exudate volume (inflammation)
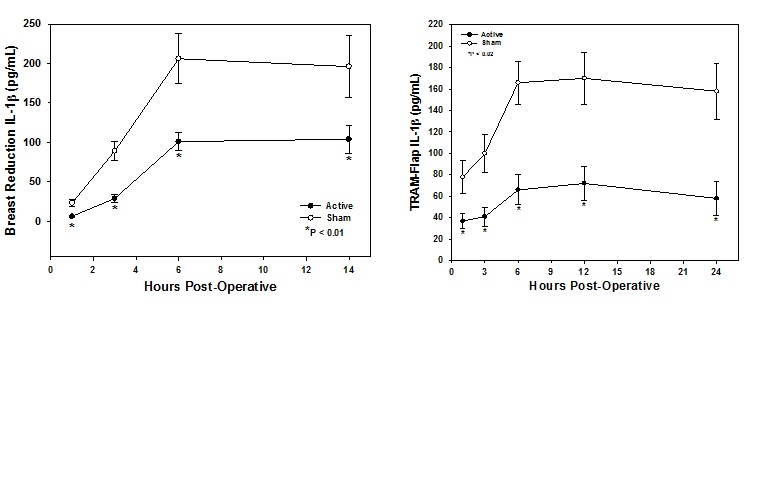
Fig 3: Effect of PEMF on Pro-Inflammatory IL-1β in wound exudates (inflammation)
Back to 2014 Annual Meeting Abstracts
|
|




