|
|
|
|
|
Back to 2014 Annual Meeting Abstracts
The Prevalence of Strabismus In Unilateral Coronal Craniosynostosis
Fares Samra, M.D., J Thomas Paliga, Youssef Tahiri, M.D., Linton A. Whitaker, M.D., Scott P. Bartlett, M.D., Brian J. Forbes, M.D., Ph.D., Jesse A. Taylor, M.D..
University of Pennsylvania and Children's Hospital of Philadelphia, Philadelphia, PA, USA.
BACKGROUND: While there is a clear correlation between unilateral coronal synostosis (UCS) and ocular motility abnormalities, the literature provides little information as to the true epidemiology of strabismus, or the underlying etiology of these paralleled pathologies. The purpose of this study is to investigate the rate of oculomotor abnormalities associated with UCS and its management.
METHODS: A retrospective review of all patients identified to have single-suture, non-syndromic UCS treated by fronto-orbital advancement at a tertiary craniofacial referral center from 1977 to 2013 was performed. Inclusion criteria mandated complete medical, surgical, and ophthalmological records. Patients were evaluated for strabismus both pre-operatively and post-operatively, and as to whether eye muscle surgery was performed. Attention was also given to the type of strabismus that was present, grouped as superior oblique palsies or horizontal strabismus.
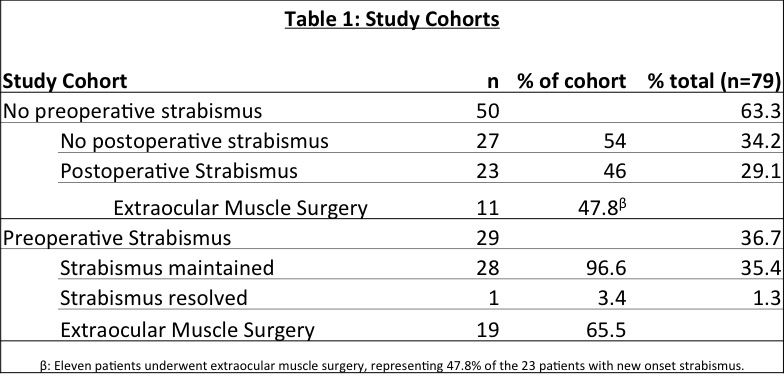
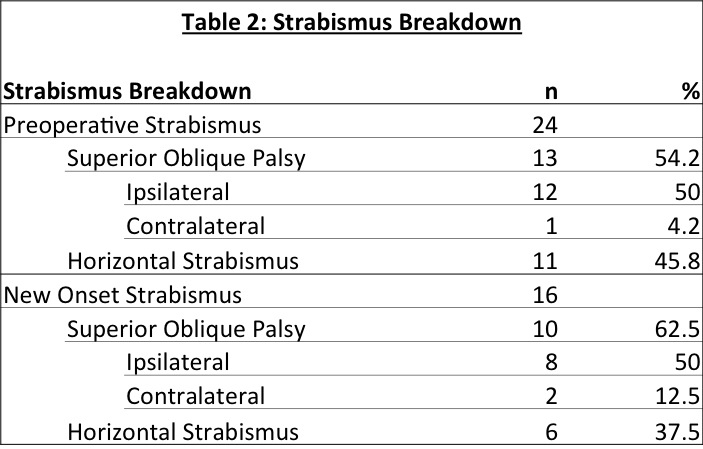
RESULTS: A total of 181 patients underwent treatment for UCS at our institution during the study period, of which 79 met the inclusion criteria. 29 patients had strabismus prior to any craniofacial surgical intervention. Following fronto-orbital advancement, 23 patients (46%) developed a new onset strabismus. 55 patients had no change in their preoperative ocular examination, and one patient had resolution of preoperative strabismus. Of the 51 patients who had postoperative strabismus, 30 went on to have eye muscle surgery. Table 1 summarizes the results of the different study cohorts. There were no statistically significant differences in gender (p=0.477), race (p=0.395), sidedness of suture involvement (p=0.552), or age at intervention (p=0.66) in comparing the group with new postoperative strabismus and those without. Comparison made between patients who had preoperative strabismus and those that developed new onset strabismus demonstrated that superior oblique palsy was the most common diagnosis in both cohorts (54.2% and 62.5%, respectively). Horizontal strabismus occurred at rates of 45.8% and 37.5%. Detailed findings are outlined in Table 2. There were no statistically significant differences in the frequency of diagnosis between the two groups.
CONCLUSIONS: This study sheds new light on the prevalence of strabismus in UCS, and more importantly, the risk of developing strabismus in the setting of conventional fronto-orbital advancement. This data will allow more accurate pre-operative counseling and reinforces the important role of ophthalmologists as members of the multidisciplinary craniofacial team.
Back to 2014 Annual Meeting Abstracts
|
|




