|
|
|
|
|
Back to 2015 Annual Meeting
Pediatric Craniofacial Fractures: National Prevalence and Management
Benjamin B. Massenburg, BA, Paymon Sanati-Mehrizy, BA, Peter J. Taub, MD.
Icahn School of Medicine at Mount Sinai, New York, NY, USA.
INTRODUCTION:
Head trauma is the most common cause of death due to injury in children, and trauma alone is the leading cause of morbidity and mortality in pediatrics. This study aimed to characterize the demographics and economic burden associated with the surgical and non-surgical repair of craniofacial fractures in the pediatric inpatient population in the United States.
METHODS:
A retrospective cohort study was performed using the 2012 Kids' Inpatient Database which identified 20,070 patients who had a skull or facial fracture, of whom 6,395 (31.9%) were treated surgically. Epidemiologic patient and hospital data were analyzed as potential determinants of surgical treatment, prolonged hospitalizations, and higher charges.
RESULTS:
Pediatric craniofacial fractures are estimated to represent \.2 billion of national healthcare expenditures annually. The average patient charge for surgical treatment of a craniofacial fracture in the pediatric population is \,849 compared to \,490 for non-surgical management (p<0.001), and the average length of stay was longer for surgical repair when compared to non-surgical management for craniofacial fractures (5.3 days vs. 4.6 days, p<0.001).
Patients who were older, African American, had non-private insurance, whose fracture was caused by external trauma, and who were treated in an urban hospital had an independently increased likelihood of surgical repair of craniofacial fractures.
Patients who were older, female, insured, of lower income brackets, whose fracture was caused by a motor vehicle accident, who had surgical treatment of their craniofacial fracture, and who were treated in hospitals in the South, Midwest, or West, teaching hospitals, and government-owned hospitals had an independent risk for a prolonged hospitalization.
Patients who were older, Caucasian, insured, whose fracture was caused by a motor vehicle accident, and who were treated in hospitals in the South, teaching hospitals, pediatric hospitals, larger hospitals, and government-owned hospitals had an independent risk for increased patient charges.
CONCLUSIONS:
Craniofacial fractures in the pediatric population represent a large economic burden to the patient and family, as well as the healthcare system as a whole. The identified patient and hospital demographics that are associated with prolonged hospitals stays and higher patient charges may represent potential barriers to care, and additional research to elucidate these factors is warranted.
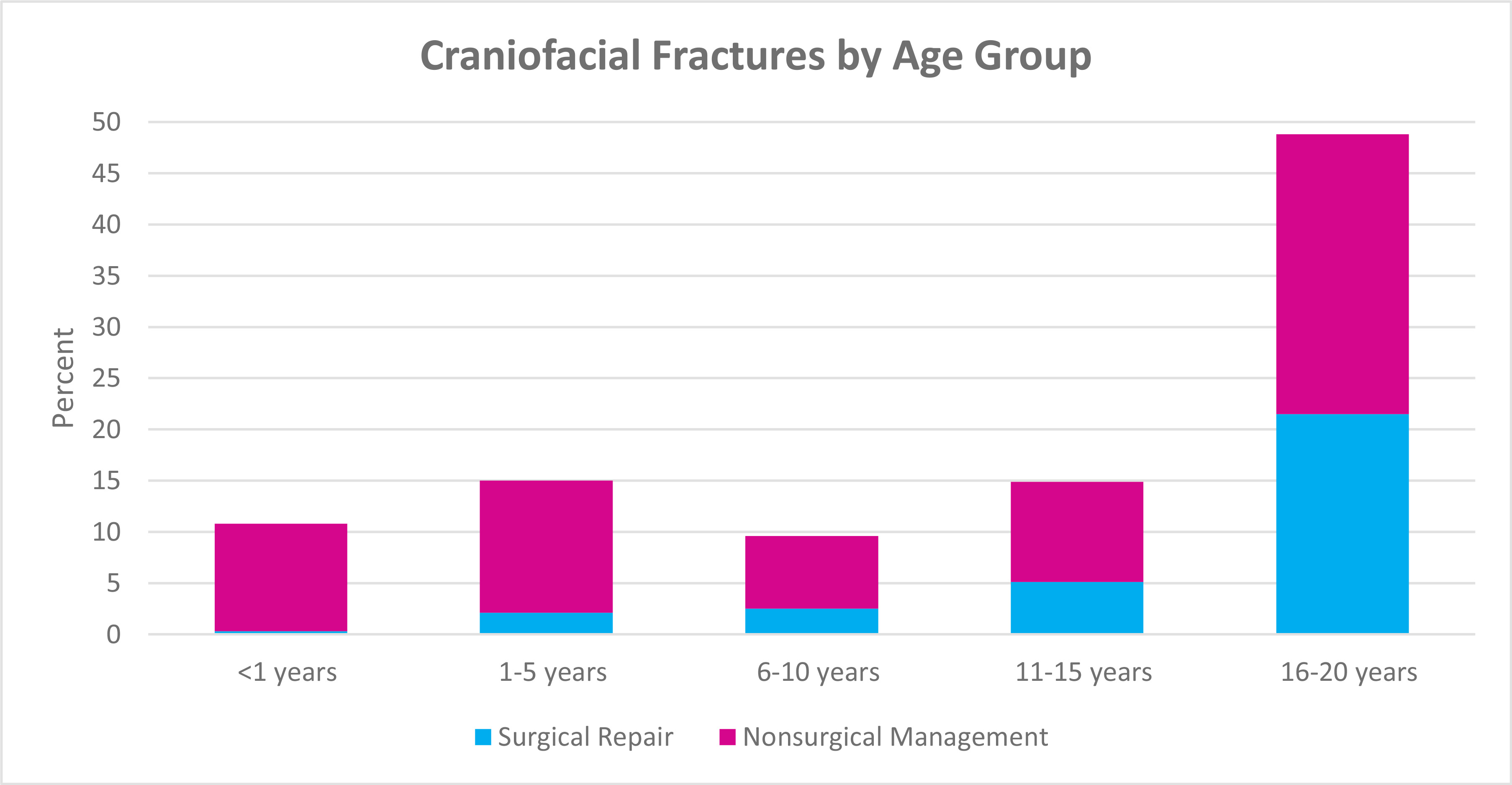
Figure 1. The incidence of craniofacial fractures and the frequency of surgical repair by age group.
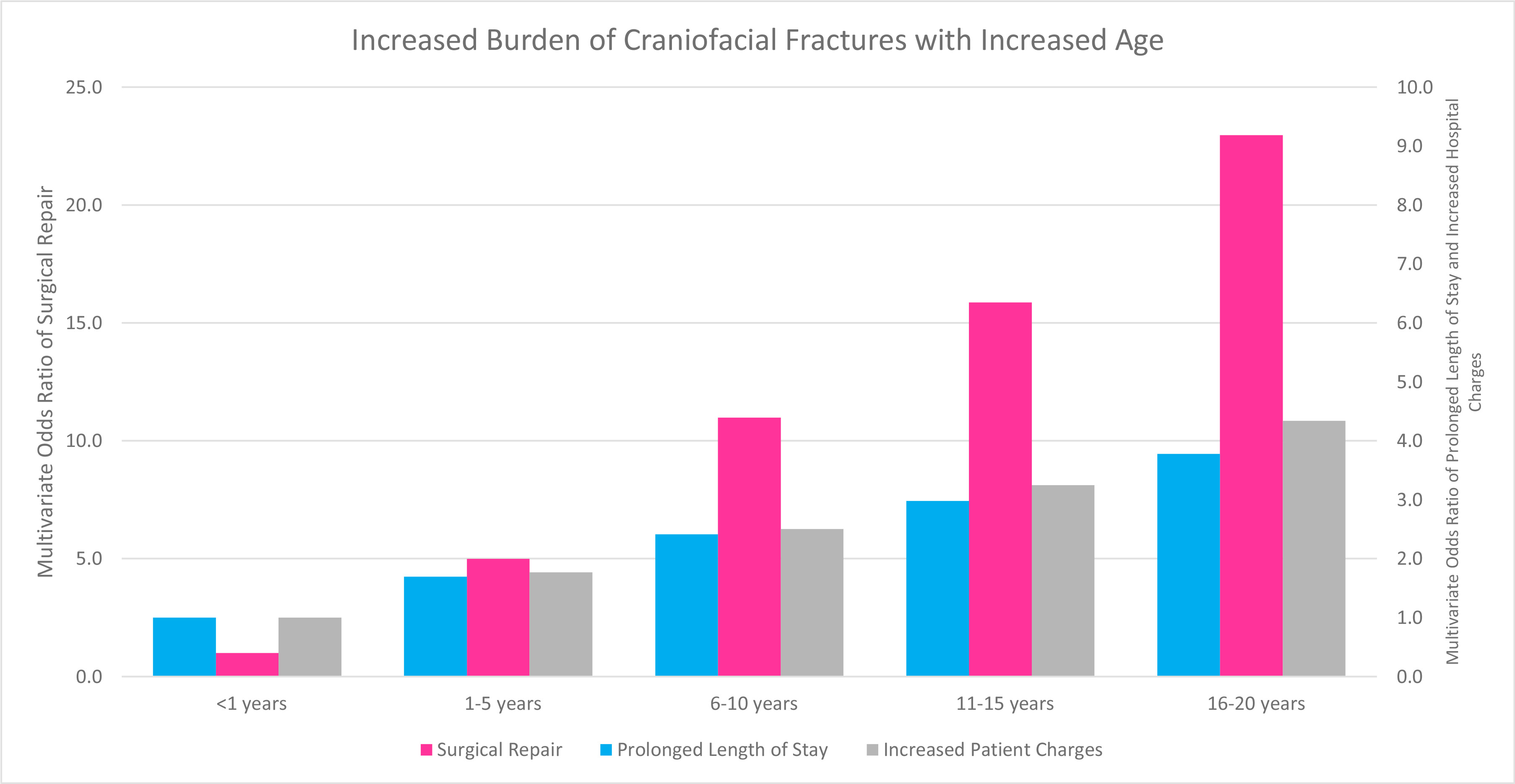
Figure 2. Increased Burden of Craniofacial Fractures with Increased Age: Multivariate Adjusted Odds Ratio with Age <1 years as the reference category.
Back to 2015 Annual Meeting
|
|




