Back to 2015 Annual Meeting
Analysis of Chimeric Free Flaps in Reconstruction of Composite Head and Neck Defects
Lin Lin Gao, MD, Liza C. Wu, MD, Marten N. Basta, MD, David Low, MD.
University of Pennsylvania Health Systems, Philadelphia, PA, USA.
Background: Composite head and neck defects present a reconstructive challenge and require more tissue offered by standard autologous free flaps. We present our institution's experience with chimeric flaps and show comparability in success, complications and costs compared with standard free flaps.
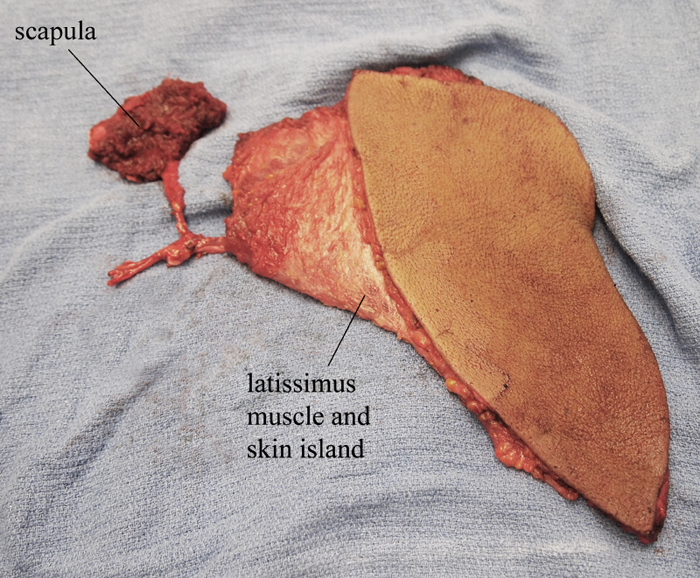
Methods: We performed retrospective cohort study and included all chimeric free flap reconstruction in our institution from 2005-2013 (Fig. 1). We identified a matched cohort of patients who underwent standard free flap reconstruction. We identified preoperative variables using univariate comparisons to allow matching.
Results: We identified twenty-five patients who underwent chimeric free flap reconstruction and found matched cohort of patients who underwent standard reconstruction. The most common indication requiring chimeric flap was squamous cell cancer resection involving the mandible (Table 1). We found the most common type of chimeric flap used was the anterior lateral thigh flap, using the facial artery and branch of internal jugular as recipient vessels (Table 2). There were no flap loss and all patients had a stable airway and were receiving enteral feeds upon discharge (Table 3). Surgical complication rate was 32% with wound infection being the most common. Medical complication rate was 16% and there were no perioperative mortality. Surgical and medical complication rates, costs and length of procedure were similar for patient cohort who underwent standard reconstruction. Use of chimeric flaps was not associated with increased complication rates.
Conclusions: For composite head and neck defects, chimeric flaps, with its dual tissue paddle and single microvascular anastomosis, provide reliable and versatile reconstruction with excellent outcomes.
Table 1. Baseline medical co-morbidities and defect characterstics | | | Age | 60.9 | | BMI | 25.2 | | Sex | | | Male | 64.0% | | Female | 36.0% | | ASA class | | | Class 2 | 32.0% | | Class 3 | 68.0% | | Smoking status (active or past) | 56.0% | | COPD | 8.0% | | CAD | 24.0% | | Length of follow up (months) | 8.9 | | Cause | | | Squamous cell cancer | 72.0% | | Osteoradionecrosis | 12.0% | | Adenoid cystic carcinoma | 12.0% | | Gun shot wound | 4.0% | | Defect involvement | | | Mandible | 48.0% | | Larynx | 20.0% | | Maxilla/Midface | 8.0% | | Other | 24.0% |
Table 2. Operative characterstics | | | Type of flap | | | ALT | 88.0% | | Parascapular | 4.0% | | Latissimus | 4.0% | | Iliac crest | 4.0% | | Recipient artery | | | Facial (End to end) | 72.0% | | External carotid (End to side) | 16.0% | | Superficial temporal (End to end) | 8.0% | | Superior thyroid (End to end) | 4.0% | | Recipient vein | | | Branch of IJ (End to end) | 68.0% | | Facial vein (End to end) | 16.0% | | IJ (End to side) | 12.0% | | Superficial temporal (End to end) | 4.0% | | Coupler Use | 88.0% | | Operating time | 9:15 | | Estimated blood loss (cc) | 394.0 | | Vasopressor requirement | 72.0% | | Intraoperative heparin drip | 16.0% |
Table 3. Outcomes and Complications | | | Flap loss (partial or full) | 0.0% | | Airway status upon discharge | | | No oxygen requirement | 28.0% | | Tracheostomy | 72.0% | | Feeding status upon discharge | | | Oral feeding | 16.0% | | Tube feeding | 84.0% | | Length of stay (days) | 8.8 | | Cost (\0 | 39354 | | Surgical complications | 32.0% | | Wound infection | 24.0% | | Fistula | 4.0% | | Hardware exposure | 4.0% | | Hematoma | 4.0% | | Medical complications | 16.0% | | Sepsis | 4.0% | | Aspiration pneumonia | 4.0% | | UTI | 4.0% | | Acute MI | 4.0% |
Back to 2015 Annual Meeting
|




