Back to 2015 Annual Meeting
A Projected 3D Image as a Topographic Guide for Fat Transfer to the Face
Jillian E. Schreiber, BA1, Carrie Stern, MD2, Evan Garfein, MD2, Katie E. Weichman, MD2, Oren Tepper, MD2.
1Albert Einstein College of Medicine, Bronx, NY, USA, 2Montefiore Medical Center, Bronx, NY, USA.
Purpose
Autologous fat transfer is a widely accepted method of facial soft-tissue augmentation for cosmetic and reconstructive purposes. Nonetheless, the planning and execution of fat transfer remains largely subjective. With the availability of 3D surface scanning, virtual surgical planning for soft-tissue augmentation is now a reality. We describe the first soft tissue virtual plan for fat transfer to the face using the novel concept of topography. The created topographic map is transferred to the patient for intra-operative guidance with the use of projection, thereby creating a 3D hologram.
Methods
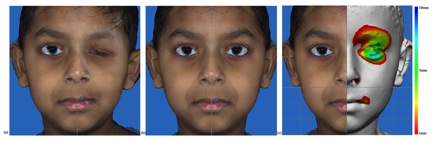
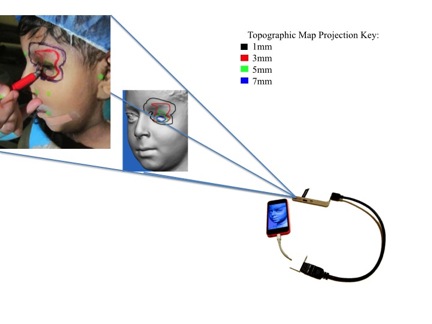
Patients undergoing AFT for facial asymmetry had 3D pre-operative surface scanning (Canfield Vectra H1). A mid-sagittal plane was used to bisect the 3D scan into two distinct hemi-faces. The reference hemiface was reflected onto the side of the defect and a color map was generated outlining the volumetric difference between surfaces (Figure 1). Tracings were made at 2mm projection intervals. The maps were uploaded onto a smart phone (iPhone) and projected using a hand-held, smart phone compatible LED Pocket Projector (axaa Technologies, USA). Colored marking pens assigned to specific projection values were used to trace the map on the patients pre-operatively (Figure 2). Fat was injected according to the region and degree of deficiency as topographically indicated.
Results
To our knowledge, this paper offers the first report of soft-tissue virtual surgical planning. This is a novel concept of pre-operative markings using 3D surface scanning and analysis, rather than surgeon judgment alone. Using 3D surface scanning and symmetry analysis with hemi-composites, we successfully demonstrated generation a topographic map of soft-tissue deficiency and transferred this virtual plan to the operating room for guidance during AFT. The virtual plan was easily projected onto the skin-surface, which guided the precise location and degree of soft-tissue augmentation needed to achieve symmetric results.
Conclusion
Topographic maps are a simplified translation of the complex three-dimensional facial contour. They provide an easy-to-follow guide tailored to the patient's unique volume needs which are often not appreciated on standard 2D photographs. Virtual surgical planning continues to be recognized as a superior method facial skeleton reconstruction, however, it has yet to be incorporated into soft tissue procedures. 3D surface scanning allows for objective analysis of the facial contour that will continue to open the door for soft tissue surgical planning. The value of this technology and its applications in plastic surgery has yet to be explored.
Figure 1. Defining the facial topography using 3D hemi-composites and color mapping of volume deficiency.
Figure 2. Projected 3D hologram to skin surface for surgical guidance.
Back to 2015 Annual Meeting
|




