|
|
|
|
|
Back to 2015 Annual Meeting
3D Scanning Provides a Novel Understanding of Arcus Marginalis Release and Tear Trough Deformity
Carrie Stern, MD1, Jillian Schreiber, BA2, Evan Garfein, MD1, Elizabeth Jelks, MD3, Glenn Jelks, MD3, Oren Tepper, MD1.
1Montefiore Medical Center, New York, NY, USA, 2Albert Einstein College of Medicine, New York, NY, USA, 3Jelks Medical, New York, NY, USA.
Purpose
Many experts believe the arcus marginalis plays a critical role in tear-trough deformity. Arcus marginalis release (AMR) is performed with fat repositioning to soften the lid-cheek junction and achieve a more youthful midface contour. The following study used 3D photography and computer analysis to document changes in the tear-trough and midface contour in response to AMR with malar lipostructure.
Methods
Cadaver specimens (n=4) underwent AMR on the right side via a transconjunctival retroseptal approach, while the left hemiface was left intact. Following this, injection of fat analogue of 2cc and 4cc to the deep medial cheek (DMC) was performed bilaterally. To analyze midface contour following lipostructure, computer-overlay of interval 3D photographs with baseline surfaces was performed and color projection maps were generated. The lower limit was set at a 1mm change from baseline. Projection was measured at points along the tear-trough for the released and non-released hemiface.
Results
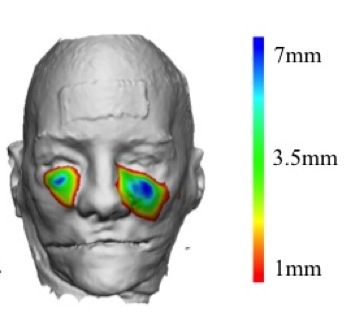
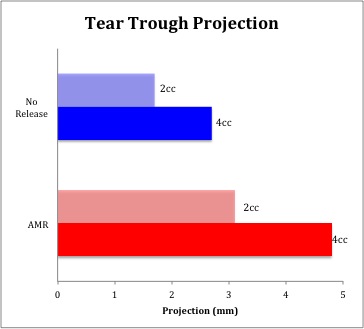
For both hemifaces, improved projection of the tear-trough was greatest at the level of the medial limbus. However, projection in the tear-trough was significantly greater with AMR compared to without. (3.1+/-0.5mm, 4.8+/-0.7mm versus 1.7+/-0.9mm, 2.7+/-1.1mm). For the non-released hemiface, the tear-trough consistently represented the superior boundary of the DMC zone of augmentation (ZOA) for all injection values. In contrast, with AMR, the ZOA was no longer restricted superiorly and extended across the tear-trough to enter the lower-lid. (Figure 1 ) Sagittal section at the medial limbus demonstrated minimal projection at the level of the tear-trough and an accentuated lid-cheek junction for the non-released hemiface, while AMR results in increasingly unified contour (Figure 2).
Conclusion
Topographical changes following lipostructure to the DMC were significantly different between the hemifaces with and without AMR. By creating an anatomical communication between the retro-orbicular space and deep malar fat compartments, lipostructure to the DMC results in softening of the lid-cheek junction and more pronounced correction of tear-trough deformity.
Legend:
Figure 1. ZOA due to DMC augmentation with AMR (right) versus no release (left).
Figure 2. Tear-trough projection following 4cc injection to DMC for alone and with AMR.
Back to 2015 Annual Meeting
|
|




