Back to 2015 Annual Meeting
Cost-Utility Analysis of Ventral Hernia Repair With a Bridging Biologic Mesh
Marten N. Basta, MD, Lin Lin Gao, MD, Stephen J. Kovach, MD, John P. Fischer, MD.
University of Pennsylvania School of Medicine, Philadelphia, PA, USA.
BACKGROUND: With long-term reported hernia recurrence ranging from 20-60%, ventral hernia repair with an interpositional bridging mesh persists as the most challenging hernia procedure. Additionally, due to the complexity of these defects and the higher levels of contamination, the majority of these repairs are performed with acellular dermal matrix. Given the expensive nature of these biologic meshes, coupled with the high complication rate, the cost of these surgeries has come under considerable scrutiny. The aim of this study was to examine the cost-utility of ventral hernia repair with a bridging biologic mesh.
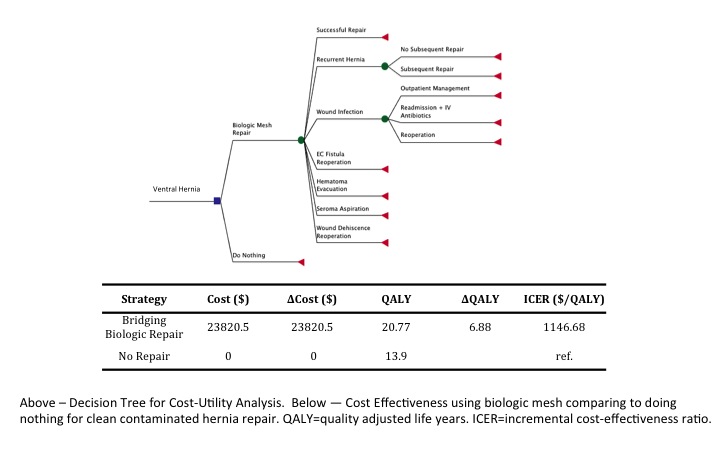
METHODS: The cost-utility analysis was comprised of 3 components: outcome (health state) probabilities, costs of each outcome, and quality of life data (or utility) for each outcome. Probabilities for common outcomes related to ventral hernia were obtained through systematic review of the literature. Only studies with a minimum of 18 months of follow-up were included. Costs for each health state were derived from national DRG reimbursements for 2013. For utility data, a prospective survey was administered to 300 nationally representative individuals to determine quality-adjusted life years (QALYs) for 14 VHR-specific health states. A decision tree was created with 2 branches, ventral hernia repaired with bridging biologic mesh versus ventral hernia without repair. Overall expected cost and QALYs for VHR were assessed using a Monte-Carlo Simulation with sensitivity analyses.
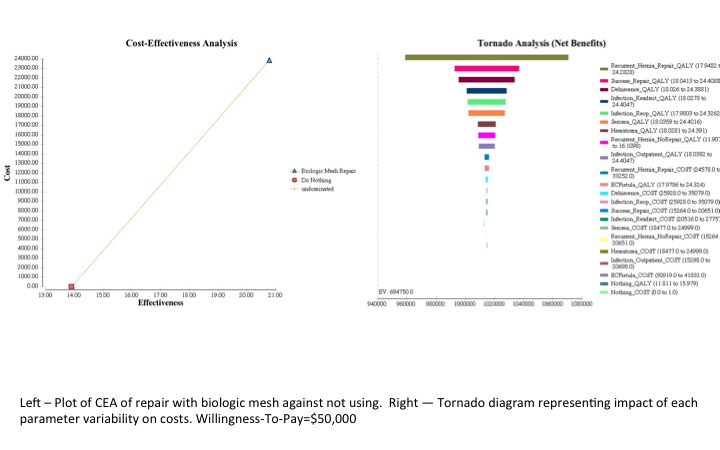
RESULTS: Bridging biologic mesh reinforcement had an expected cost of \,821 and QALY gained of 20.77. The reference situation, ventral hernia without repair, had an expected cost of \C:\inetpub\wwwroot\WebsiteHosting\NESPS\www.nesps.org\meeting\abstracts\2015\82.cgi and QALY of 13.90. Compared to unrepaired ventral hernia, the Incremental Cost-Efficacy Ratio (ICER) for bridging biologic mesh repair was 1,147 \
QALY. Univariate and multivariate sensitivity analysis with a willingness-to-pay (WTP) threshold of \,000/QALY demonstrated robustness of the results, as no parameter altered the conclusion that bridging biologic mesh, despite the relatively high complication incidence, remains cost-effective compared to a ventral hernia that is not repaired. Finally, WTP threshold was varied from 0 to \,000/QALY and it was found that bridging biologic mesh repair was most commonly the optimal strategy across all WTP thresholds.
CONCLUSIONS: This study demonstrates that bridging biologic mesh ventral hernia repair, compared to no repair, is the more optimal choice regarding cost-utility. Despite the high cost of biologic mesh, these findings may facilitate clinical decision-making in the approach of these particularly complex ventral hernia defects.
Back to 2015 Annual Meeting
|




