Back to 2015 Annual Meeting
Revisiting The Reverse Posterior Tibial Artery Fasciocutaneous Flap: An Anatomic Study of Retrograde Venous Flow and Its Clinical Application
Dylan Perry, BA, Mark G. Albert, MD, Angela Ferris, BS, Raymond M. Dunn, MD.
University of Massachusetts, Worcester, MA, USA.
BACKGROUND
Flap necrosis is common in lower extremity perforator based fasciocutaneous flaps where skin islands have been designed to exceed the physiologic vascular territory of involved perforators. To avoid this problem, we have utilized wide flap territories including multiple perforators, while sacrificing the axial (posterior tibial) artery where necessary and clinically indicated. The arterial anatomy of the posterior tibial artery perforators has been well delineated in previous studies. In 1997, Nakajima et. al. examined the venous flow from the radial forearm and anterior tibial reverse flaps.
METHODS
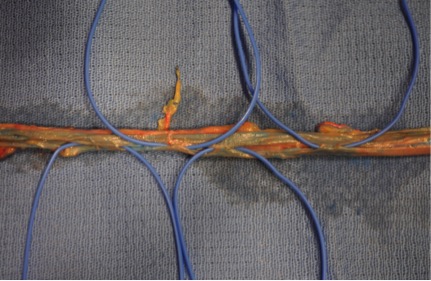
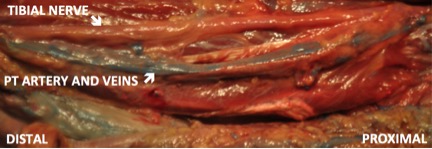
An anatomic study was performed using lightly embalmed cadavers (n=6) to demonstrate the venous flow from the posterior tibial artery fasciocutaneous flap. A cutdown was performed at the medial ankle and popliteal fossa and latex was injected through the posterior tibial artery and veins in a retrograde fashion to simulate the flap's retrograde flow. The posterior tibial vessels were then dissected and bridging veins were identified. The relationship of these vessels to each other and to the tibial nerve was then examined. Two clinical cases are presented involving the use of the reverse posterior tibial artery flap for coverage of lower extremity defects.
RESULTS
Results demonstrate distinct interconnections between the two posterior tibial veins and non-parallel offset of venous valves. None of the interconnections cross-over or involve the tibial nerve. In our three clinical cases, we experienced no flap viability complications despite using skin islands in excess of those that would satisfactorily be supplied by a single perforator. There was no indication of extremity arterial insufficiency following the sacrifice of the posterior tibial artery. At six months follow-up, the reverse posterior tibial flap provided durable non-edematous coverage of our lower extremity defects.
CONCLUSIONS
This cadaveric study has defined the bridging and communicating veins that connect the posterior tibial vena-comitantes. The reverse posterior tibial artery flap can safely be elevated with its entire venous system without injury to the tibial nerve and be performed without consequence to lower extremity vascularity in appropriate clinical cases.
Back to 2015 Annual Meeting
|




