|
|
|
|
|
Back to 2015 Annual Meeting
Perioperative Management for Microvascular Free Tissue Transfer: A Pilot Study Examining the Utility of a Checklist in Improviang Communication Between Microsurgeons and Anesthesiologists
Inzhili K. Ismail, MD1, Richard Agag, MD1, Ashit Patel, MD1, Kristen Rezak, MD1, Stacey Burns, BS, MBA2.
1Albany Medical Center, Albany, NY, USA, 2Albany Medical College, Albany, NY, USA.
BACKGROUND: Free tissue transfer procedures are complex, therefore communication between anesthesiologists and microsurgeons is essential. The pre-operative surgical checklist has been shown to decrease complications (1, 2), but a checklist specific to free tissue transfer cases has not been described. Evidence-based guidelines for intraoperative management of free flaps were developed (3), and used to produce a pre-operative checklist (Figure 1). Our goal is to evaluate if a checklist guiding perioperative management for free flap procedures improves communication and adherence to evidence-based guidelines.
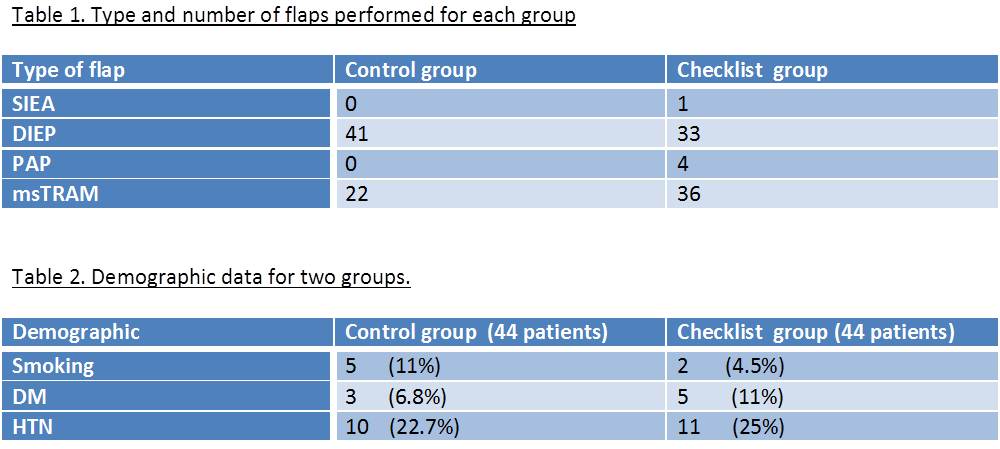
METHODS: Patients who underwent breast reconstruction with free tissue transfer between January 2011 and February 2015 were selected for this study. Forty-four (checklist group) underwent free tissue transfer after the microsurgeon and the anesthesiologist had a directed pre-operative discussion following the items detailed in the checklist. Forty-four matched patients, retrospectively selected as controls, had undergone free flaps without a checklist guided discussion. Anesthesia records were reviewed retrospectively for data on core temperature range, crystalloid administration, urine output and use of vasopressors. 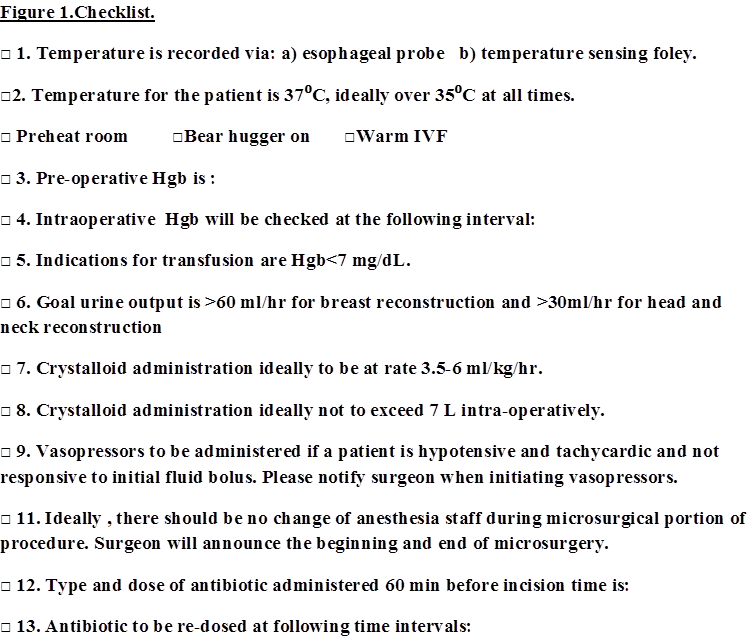
RESULTS: A total of 88 patients were included in the study, and a total of 140 free flaps were performed (Table 1). Mean age was 50.7 for the checklist group and 47.5 for the control group. Seventy-three percent of the checklist group had crystalloid administration in recommended range of 3.5cc/kg/hr-6 cc/kg/hr. However, 41% of the control group had crystalloid administration in the recommended range (p=0.0022). Overall, 41 % of the patients in the control group received IVF in excess of 7L intra-operatively vs. 15 % of patients in the checklist group (p=0.0046). Mean core body temperature was less than 35C° in 18% control group patients vs. 4.5% checklist group of patients (p=0.0027). Finally, vasopressors were used in 27.2% of patients in both control and checklist group. However, in the checklist group, the type and timing of vasopressor use was always discussed with the microsurgeon, whereas this occurred in 14% of the control group (p<0.0001).
CONCLUSIONS: Our pilot study demonstrates that a pre-operative checklist guiding intraoperative management ensures critical communication between microsurgeons and anesthesiologists, leading to appropriate vasopressor use, decreasing excessive crystalloid administration and maintaining recommended body temperature. While further studies are necessary to determine the impact on outcomes, we believe that a checklist, as described, is an essential tool in free tissue transfer procedures.
References:
1.WHO Surgery Safety Checklist ( Accessed April, 2015 at http://www.who.int/patientsafety/safesurgery/checklist/en)
2.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009, 360:491-99.
3.Motakef S, Mountziaris PA, Ismail IK, Agag RL, Patel A. Emerging paradigms in perioperative management for microsurgical free tissue transfer: review of literature and evidence based guidelines. Plast Reconst Surg. 2015, 135(1):290-299
Back to 2015 Annual Meeting
|
|




