Back to 2016 Annual Meeting
Optimizing results in patients with glandular ptosis undergoing nipple-preserving mastectomy and immediate two-stage implant-based breast reconstruction
Andreas M. Lamelas, MD, Eric M. Jablonka, M.D., Cara L. O'Neill, PA-C, MS, Samantha R. Rogalski, PA-C, MS, Mark L. Smith, MD, FACS, Mark R. Sultan, MD, William Samson, MD, FACS.
Mount Sinai Medical Center, New York, NY, USA.
Background: Glandular breast ptosis presents unique challenges in patients undergoing nipple-preserving mastectomy and implant reconstruction. This often results with superior malposition of the nipple, relative to the implant. Standard radial and inframammary crease (IMC) incisions do not address the vertical skin excess in the lower pole. In addition, standard IMC incisions may not provide optimal exposure for performing the mastectomy in this breast morphology.
Methods: The technique presented utilizes a long transverse incision at an intermediate distance between the NAC and the IMC. The skin below the incision is de-epithelialized and sutured to the freed inferior margin of the pectoralis major muscle serving as an internal vascularized flap to support the lower pole of the prosthesis. ADM may also be interposed between the dermal flap and muscle as indicated. This technique affords several advantages:
1. Reduces lower pole vertical skin excess, optimizing nipple position relative to the prosthesis.
2. Shortens the length of the superior skin flap, decreasing the risk of distal skin flap necrosis.
3. Conceals the final scar along the IMC.
4. Provides vascularized coverage of the prosthesis under the most distal aspect of the upper breast skin flap.
5. Provides the oncologic surgeon with excellent exposure to perform the mastectomy.
6. Optimizes initial expander fill volume.
Results: Seven consecutive patients (13 breasts) underwent this procedure by the senior author. Five patients had primary pseudoptosis and two patients had secondary pseudoptosis, resulting from prior breast reduction. Average patient age was 45 and BMI was 22.7. Average percent of maximum expander fill volume intra-operatively was 76.1%. In three patients (5 breasts) ADM was used as an interposition between the dermal flap and the pectoralis muscle. There were no infections, implant exposures/loss, or reoperations for skin necrosis. One patient/breast developed minor nipple epidermolysis, which healed spontaneously. All patients went on to have permanent implants placed.
Conclusions: This technique is a safe and effective method for addressing glandular ptosis in patients undergoing nipple-preserving mastectomy and immediate two-stage implant-based reconstruction. 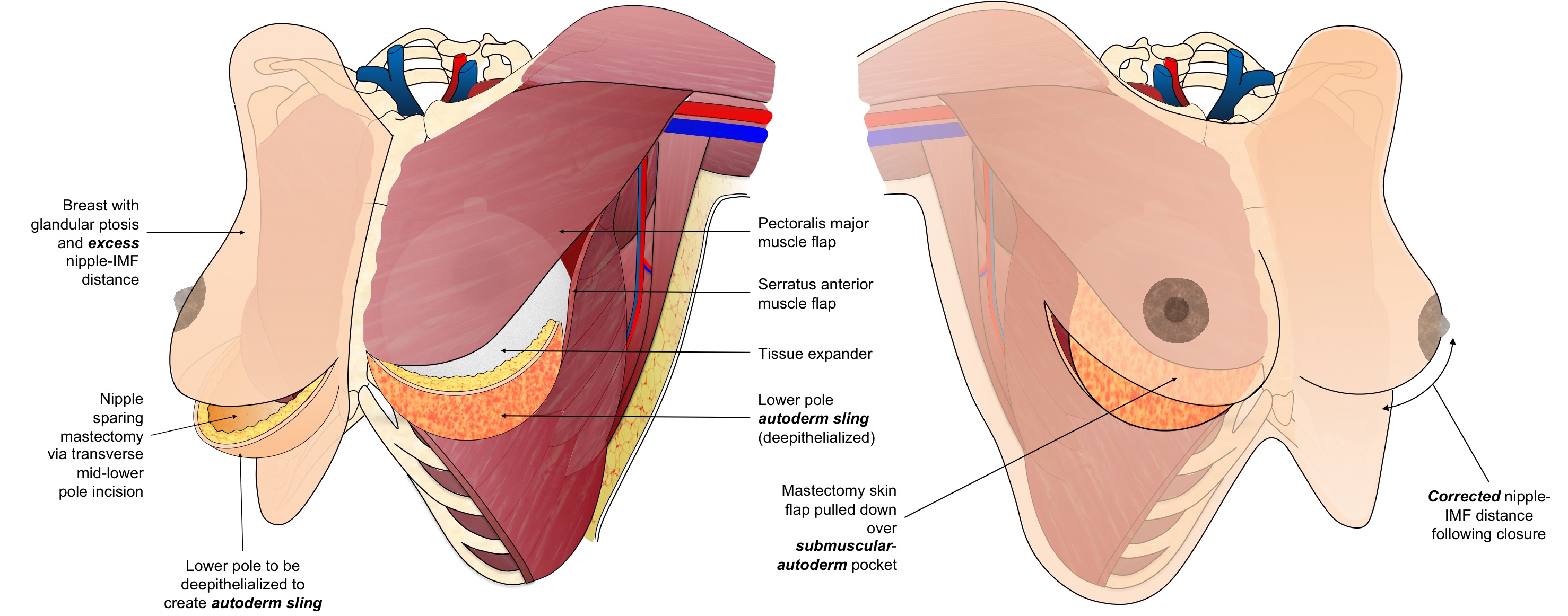  
Back to 2016 Annual Meeting
|
