Back to 2016 Annual Meeting
Ophthalmic Injuries and Timing of Surgical Intervention in Pediatric Orbital Fractures
Devin Coon, M.D., Martin Kosztowski, M.D., Richard Redett, M.D., Michael P. Grant, M.D., Ph.D..
Johns Hopkins University, Baltimore, MD, USA.
BACKGROUND: Pediatric orbital fractures represent a challenging clinical problem. In particular, there is virtually no data on concomitant ophthalmic injury during orbital fractures in children. We sought to assess these patients at a state-designated ophthalmology referral center to develop guidelines for surgical timing and how to safely manage orbital fractures if eye injuries are present.
METHODS: This was a cohort study reviewing the Johns Hopkins/Wilmer Eye experience over a ten year period. Children who did not undergo a full ophthalmic examination or never returned for follow-up were excluded. Patients were assessed at follow-up for globe malposition, ophthalmic pathology and complications. Univariate logistic regression was used for exploratory analysis. Multivariate logistic regression was used to control for potential confounders (model inclusion threshold p<0.10) to identify significant predictors.
RESULTS: One-hundred and fifty patients from the age of 0-17 years who presented with orbital fractures but without other facial fractures or trauma were included. Anterior segment pathology (traumatic iritis, corneal abrasions, or hyphema) was seen in thirty-three patients (22%). Posterior segment pathology (vitreous hemorrhage, commotio retinae, retrobulbar hematoma or optic neuropathy) occurred in thirty-two patients (21%).
Patients complaining of diplopia were much likelier to have evidence of muscle entrapment on CT imaging (p<0.001; OR 6.4) as were patients who had EOM restriction on exam (p<0.001; OR 16.8). VA of 20/40 or worse on presentation was a finding relatively specific for the presence of anterior/posterior segment injuries (sensitivity 34.1%; specificity 91.4%; 95% CIs 20.5%-49.9% and 83.8%-96.2%).
107 patients (71%) underwent fracture surgery. Thirty-nine patients (37%) had surgery within the first 48 hours; 53% had surgery between 2-21 days, while eleven (10%) underwent delayed repair (median 49 days). The overall surgical complication rate was 4.7%. Two patients had 20/40 vision or worse at the conclusion of follow-up. Presenting with any posterior segment injury (OR 10.7; p=0.006; 95% CI 2.0-58.4), retinal commotio (OR 7.3; p=0.01; 95% CI 1.5-34.8) and afferent pupillary defect (OR 28.2; p=0.002; 95% CI 3.3-242.9) were predictors of a poor outcome.
CONCLUSIONS: Management of orbital fractures in the pediatric population can be safely accomplished in the presence of ophthalmic pathology. Fractures are preferentially repaired in the one to three week window unless evidence of entrapment is present. However, we suggest that retinal/posterior segment injuries generally represent contraindications to surgery in this window. In contrast, hyphema is relatively common but can be managed by serial examination until it clears, at which time intervention can be performed. With this approach, good outcomes in visual acuity and globe position can be obtained safely.
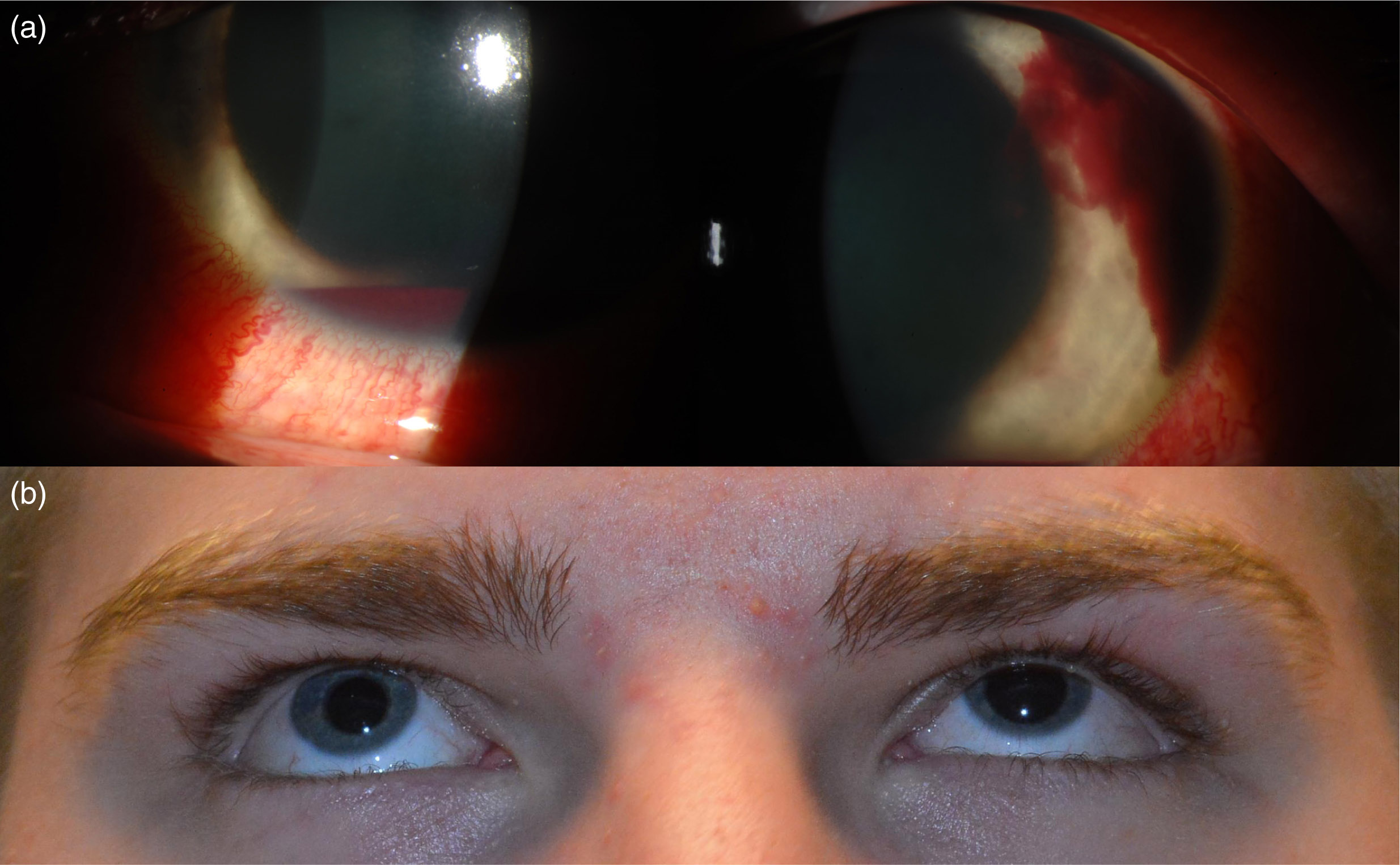
Figure 1. A 16 year-old boy struck in the eye by a baseball, sustaining an entrapped orbital floor fracture and large hyphema (a). Maximal intraocular pressure control measures were instituted and the fracture was repaired on POD 1. At two-month followup the patient retained 20/20 vision with hyphema resolution and full EOMs (b).
Back to 2016 Annual Meeting
|
