|
|
|
|
|
Back to 2016 Annual Meeting
Chemical Component Separation: A Systematic Review and Meta-Analysis of Botulinum Toxin for Management of Ventral Hernia
Michael A. Lanni, BS, Michael G. Tecce, DO, Jason M. Weissler, MD, Valeriy Shubinets, Martin J. Carney, BS, John P. Fischer, MD.
University of Pennsylvania, Philadelphia, PA, USA.
BACKGROUND: At the rate of nearly 350,000 repairs per year costing $3.2 billion, ventral hernia represents a significant surgical challenge plagued by high morbidity and recurrence rates. The most difficult ventral hernias are associated with severe lateral retraction and tension of abdominal wall muscles, often prohibiting autologous closure of the defect. Botulinum toxin (BTX) has recently been gaining popularity as a preoperative means to not only counteract abdominal wall tension, but also reduce hernia size and aid fascial closure at the time of hernia repair. This systematic review and meta-analysis evaluates reported outcomes associated with BTX injections in the setting of ventral hernia and identifies opportunities to leverage this mainstream aesthetic technology for novel use abdominal wall reconstruction.
METHODS: A literature review was conducted in accordance with PRISMA guidelines using MeSH terms “ventral hernia”, “herniorrhaphy”, “hernia repair”, and “botulinum toxins”. Qualitative studies were included for understanding high-level themes demonstrated across the literature. Relevant empirical studies from single institutions reporting pre- and post-injection data were included for meta-analysis. Outcomes of interest included changes in hernia defect width and lateral abdominal muscle length, hernia recurrence, complications, and length of follow-up.
RESULTS: Of 133 unique results, 11 publications were included for review. Many studies considered BTX to be an important adjunct to hernia repair. Two studies reported on the efficacy of BTX as a postoperative analgesic measure and one animal model reported its potential for reducing the risk of incisional hernia after laparotomy (Table 1). Three studies met criteria for quantitative analysis, involving 56 patients (Table 2). Meta-analysis revealed significant reduction of hernia width following BTX injections (mean=5.79 cm; n=29; p<0.001) and increase in length of lateral abdominal wall muscles (mean=3.33 cm; n=44; p<0.001) (Figure 1). Following hernia repair, the overall reported complications rate was 5.6%, although no complications were specifically related to the BTX use. The fascial closure rate was 100% and no hernia recurrences were noted. Mean length of follow-up was 24.7 months (range 9-49).
CONCLUSIONS: BTX appears to have tremendous potential in ventral hernia management by reducing hernia width and lengthening lateral abdominal wall muscles prior to repair. Subsequent hernia repairs demonstrated no recurrences and a low risk profile. Current evidence presents an excellent opportunity to bridge the evidence gap in preoperative practice measures for risk reduction in ventral hernia. Further studies are needed to determine the role of BTX in management of ventral hernias in addition to its efficacy in reducing incisional hernia and as a post-operative analgesic adjunct and assessment of quality of life outcomes.
Table 1. Qualitative Studies| Trial | Year | Design | Methods | Findings | | Smoot | 2009 | Prospective | Case report BTX (300 U) injected on POD 20 for pain control after VHR | Pain reduced from 10/10 to 2/10 five days after BTX injection and lasted through 3 months’ follow up | | Zielinski | 2013 | Retrospective | Describes BTX (300 U) injection technique and series of 18 patients injected with BTX prior to OA management | Reported rates of primary (83%) and partial (6%) fascial closure, planned ventral hernia (11%), complications (67%), and mortality (11%) | | Zandejas | 2013 | Retrospective | Compared postoperative opioid use (ME), reported pain, and complications in 22 patients with pre-IHR BTX (300 U) to 66 matched controls | Preoperative BTX was associated with significantly less opioid use and less pain postoperatively; No difference in LOS or complications (including opioid-related) | | Chavez-Tostado | 2014 | Retrospective | Describes BTX (100U) effect in series of 14 patients with various hernia types (i.e. midline, umbilical, flank) | Statistically insignificant decreases in defect diameter and area; complication rate of 28.6%; no recurrences | | Alam | 2016 | Review | Identified 102 unique studies from PubMed and Embase after searching for botulinum toxin, PPP, or tissue expander use in ventral hernia | Analyzed pooled data from 21 included reviews or case series; 15 PPP studies, 4 tissue expander studies, and 2 BTX studies with fascial closure rates of 84%, 92.9%, and 100%, respectively | | Cakmak | 2006 | Animal Model | Compared saline expansion volumes required to reach set intraabdominal pressure at two time points in BTX (10 U) injected rats and control rats | Post-BTX rats required 119% of their baseline expansion volume while control rats required 100.9% of theirs to reach the same intraabdominal pressure | | Lien | 2015 | Animal Model | Compared IH incidence due to tissue expander inflation 14 days after laparotomy between 3 groups: sham (no laparotomy); BTX (injected on POD0); and saline (injected on POD0) | No hernias in sham rats; rostral hernias developed in all saline and BTX rats (BTX rats’ were 43% narrower; p<0.05); 50% less BTX rats developed any caudal hernias compared to saline rats | | Rodriguez-Ruiz | 2015 | Animal Model | Compared abdominal wall tension after planned VH between BTX and control rats | No difference in VH size between groups; On VH reduction, BTX rats had less tension on the right and left abdominal walls (p<0.001;p<0.001) | | BTX, botulinum toxin A; VHR, ventral hernia repair; PPP, progressive preoperative pneumoperitoneum; IHR, incisional hernia repair; ME, morphine equivalents; LOS, length of stay; OA, open abdomen; VH, ventral hernia; POD, postoperative day | Table 2. Quantitative Studies| Trial | Year | Design | Methods | N | Δ Defect Width | Δ RAM Length | Δ LAM Length | Follow-Up | Findings | | Ibarra-Hurtado | 2009 | Prospective | Compared pre- and post-BTX (500 U) hernia dimensions via CT or clinical exam in patients prior to open VHR | 12 | -6.62 cm | Not Reported | Not Reported | 9.1 months | Pre-BTX mean defect width of 13.9 cm; mean reduction of 5.25 cm (p < 0.001); no recurrences | | Ibarra-Hurtado | 2014 | Prospective | Compared pre- and post-BTX (500 U) hernia defect and lateral abdominal muscle dimensions via CT in patients prior to open VHR | 17 | -4.97 cm | 2.59 cm | 2.44 cm | 49 months | Bilateral reduction in muscle thickness and increase in muscle length (p < 0.001; p < 0.001); pre-BTX mean defect width of 14.65 cm; mean defect reduction of 4.79 cm (p < 0.001); no recurrences | | Elstner | 2016 | Prospective | Analyzed BTX (300 U) effect on lateral abdominal muscle dimensions via CT in patients prior to laparoscopic VHR | 27 | Not Reported | 4.2 cm | 4.1 cm | 16 months | Increased lateral muscle length (p < 0.001) and up to 58% reduction in hernia defect size | | BTX, botulinum toxin A; Δ, delta; RAM, right abdominal wall muscle; LAM, left abdominal wall muscle | 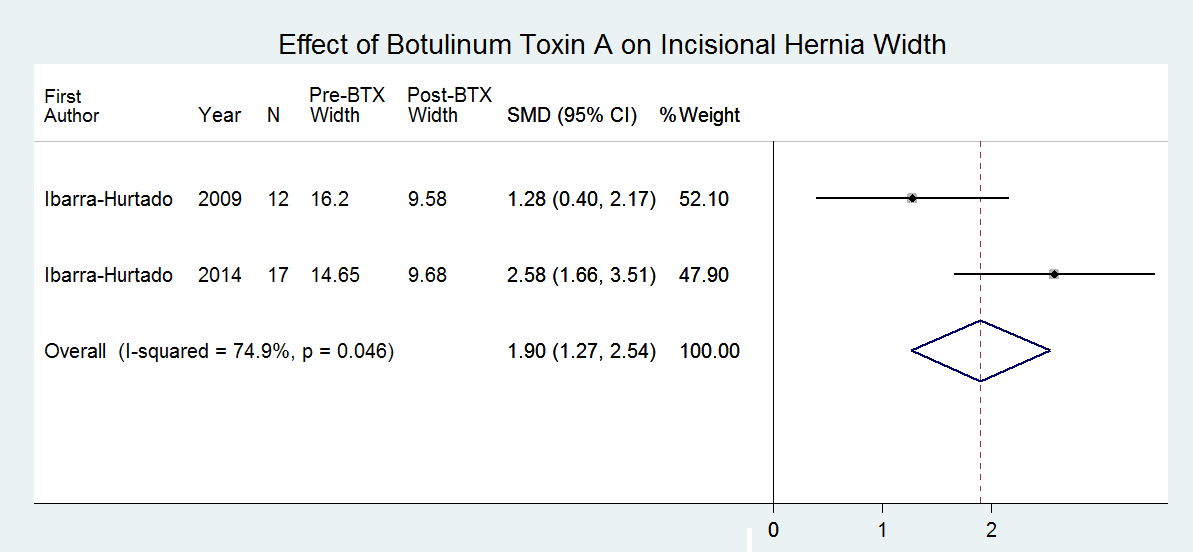
Back to 2016 Annual Meeting
|
|
