|
|
|
|
|
Back to 2016 Annual Meeting
Pelvic Surgery and Concurrent Panniculectomy: A Safe Approach for a High Risk Population
Michael A. Plastini, MD1, Daniel Eisman, BA2, Jordan Kaplan, BS2, Atlee M. Melilo, BS2, Dorothy Bird, MD1, Leilani Fahey, MD1, Martha S. Matthews, MD1.
1Cooper University Hospital, Camden, NJ, USA, 2Cooper Medical School of Rowan University, Camden, NJ, USA.
BACKGROUNG:
Previous studies have reported conflicting results as to the benefit and safety of concurrent panniculectomy and pelvic surgery. The purpose of this study is to evaluate the outcomes of patients who underwent pelvic surgery with and without concurrent panniculectomy.
METHODS:
This study utilized a single institution, retrospective chart review of women who underwent open pelvic surgery (PS) with and without concurrent panniculectomy (PAN) between January 2009 and March 2015. First, patients in the combined procedure group (PS+PAN) were identified, then they were matched with patients in the pelvic surgery group (PS) for month of procedure, age, and CPT code. The intraabdominal portion of the procedure was performed by gynecology or gynecology oncology, while plastic surgeons performed the panniculectomy for the combined cases. Patients who received a panniculectomy were referred by their gynecologic surgeon because of concerns that the size of the panniculus could interfere with pelvic access and severe intertrigo might lead to wound healing problems.
RESULTS:
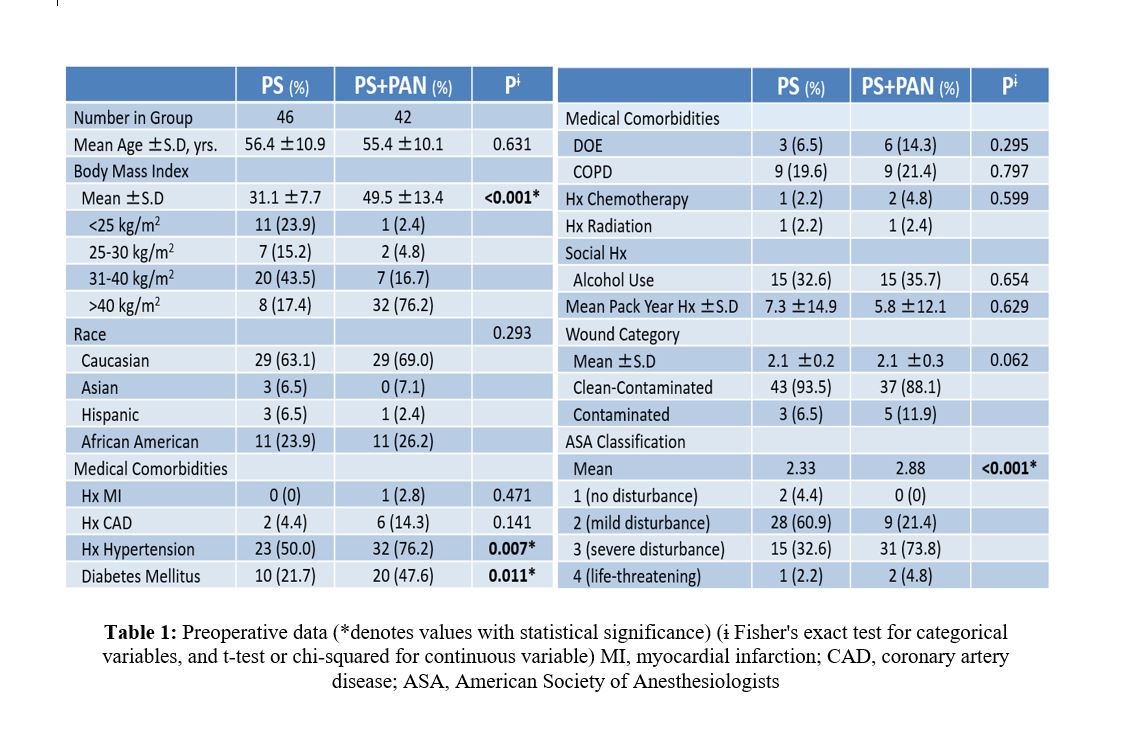
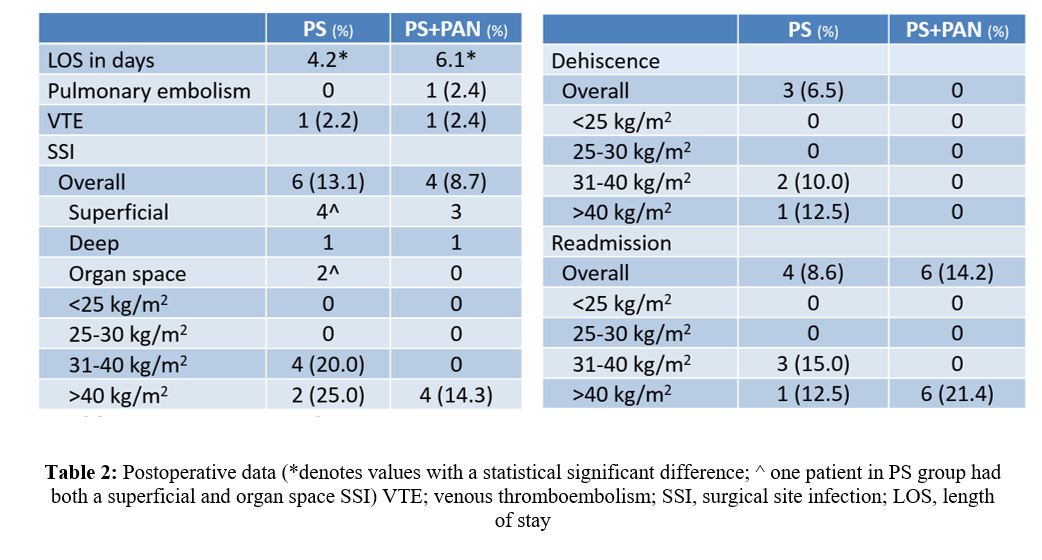
Complete data was available for forty-two of the 103 patients who underwent concurrent PS and PAN (PS+PAN) during the inclusion period. Forty-six patients were included in the PS alone group. The PS+PAN group exhibited significantly increased BMI (49.5±13.4 versus 32.1±7.7, P<0.001), ASA classification (p<0.001), rate of diabetes mellitus (p=0.011), and rate of hypertension (p=0.006) when compared to the PS group pre-operatively (Tab. 1). The PS+PAN group also had significantly increased operative time (258.9 ±20.9SEM min. vs 142.8±14.6SEM min., p<0.001) while exhibiting a trend towards decreased blood loss (381.9 versus 405.1 ml) (Fig. 1) and injury to adjacent structures (4.8% versus 8.7%) when compared to the PS group. Multiple outcomes including venous thromboembolism (VTE), pneumonia, myocardial infarction, and return to OR rates were compared between PS+PAN and PS groups, with no significant differences demonstrated between the two groups. Furthermore, the PS+PAN group exhibited a trend towards decreased surgical site infection incidence (9.5% versus 13.1%) and wound dehiscence (0.0% versus 6.5%) when compared to the PS group. As BMI increased there was a trend towards increased complications in both groups (Tab. 2).
CONCLUSIONS:
Though the PS+PAN group exhibited a significantly higher rate of risk factors when compared to the PS alone group, there was a trend towards decreased intra-operative and post-operative complications. Furthermore, PS+PAN group had no significantly increased rate of any postoperative complication including VTE as seen in previous studies. Our findings reveal that concurrent pelvic surgery and panniculectomy is a safe option that affords risk reduction for a high-risk population.
Back to 2016 Annual Meeting
|
|
