|
|
|
|
|
Back to 2016 Annual Meeting
The Current State of Prophylactic Mesh Augmentation: Outcomes, Risk Modeling, Barriers to Adoption, and the Future of Risk Reductive Surgery
Michael A. Lanni, BS, Michael G. Tecce, DO, Valeriy Shubinets, MD, Michael N. Mirzabeigi, MD, Joseph M. Serletti, MD, John P. Fischer, MD.
University of Pennsylvania, Philadelphia, PA, USA.
BACKGROUND: With the high incidence and insufficient treatments leading to disproportionately high morbidity and cost associated with the incisional hernia after laparotomy, it is crucial to investigate hernia prevention. Prophylactic mesh augmentation (PMA) is the implantation of mesh at index laparotomy to decrease a patient’s risk for developing incisional hernia (IH). The current body of evidence lacks standard guidelines for patient selection, mesh placement, and material choice. The purpose of this study is to identify areas of research needed to formulate a clinical framework and to foster responsible and appropriate of use of new technology and surgical techniques.
METHODS: We conducted a comprehensive literature search of Scopus and PubMed and a search of clinicaltrials.gov for articles and trials related to using PMA for incisional hernia risk reduction. Our review was further supplemented by including select papers on biomechanical properties of mesh, animal models, cost-practicality, patient-reported outcomes, risk-modeling, surgical techniques, and available materials related to PMA.
RESULTS: Review of 551 unique articles and 357 trials yielded numerous empirical studies (Table 1).Various options exist for mesh placement (Figure 1). Advantages and drawbacks of different mesh locations and types must be carefully considered (Tables 2 and 3). Multiple studies report that there was significant decrease in IH incidence with PMA compared to suture closure, although seromas have been associated with onlay mesh positioning. No multicenter randomized control trial (MCRCT) has been conducted in the United States to date. Only two such trials are currently active, but they are inconsistent in examining PMA variables or defining IH.
Table 1. Literature review results for PMA trials and comparative studies| Author and Setting | Study Period | Design | Details | Conclusions | | Bevis 2010 UK | 2003-2007 | RCT n=85 | Retrorectus, Polypropylene | PMA reduced the rate of IH after open AAA repair without increasing the rate ofcomplications (p=0.002) | | Llaguna 2011 USA | 2005-2007 | Comparative n=134 | Retrorectus, Biologic | PMA appears to reduce the incidence of IH in patients with multiple risk factors forIH (p=0.014) | | Bali 2015 Greece | 2007-2009 | RCT n=40 | Onlay, Biologic | PMA during AAA repair showed effectiveness and low complication rate inpreventing IH (p< 0.008) laparotomies is feasible for the prevention of IH withoutadding a substantial morbidity, even in the presence of contamination or infections(p=0.0001) | | Argudo 2014 Spain | 2009-2010 | Comparative n=266 | Onlay, Partially Absorbable | PMA for closure of emergency midline laparotomies is feasible for the prevention ofIH without adding a substantial morbidity, even in the presence of contamination orinfections (p=0.0001) | | García-Ureña 2015 Spain | 2009-2011 | RCT n=107 | Onlay, Polypropylene | Only PMA decreases the incidence of IH without adding morbidity (p=0.011) | | CaroTarrago 2014 Spain | 2009-2012 | RCT n=160 | Onlay, Polypropylene | PMA prevents IH independently of other factors (p< 0.0001) | | Timmermans 2015 Netherlands | 2009-2012 | RCT n=480 | Onlay and Retrorectus, Polypropylene | Shorttermresults show PMA can be considered a safe procedure an increase inseroma formation after onlay placement, but no increased risk of surgical siteinfection | | PREBIOUS Spain | Active | MCRCT Anticipated n=435 | Biologic | Primary outcome is incisional hernia occurrence after 2 years postoperatively.Secondary outcomes include postoperative complications, pain, and quality of life. | | PRIMA Trial Netherlands | Active | MCRTC Anticipated n=435 | Onlay and Retrorectus, Polypropylene | Primary outcome is incisional hernia occurrence after 2 years postoperatively.Secondary outcomes include postoperative complications, pain, and quality of life. | 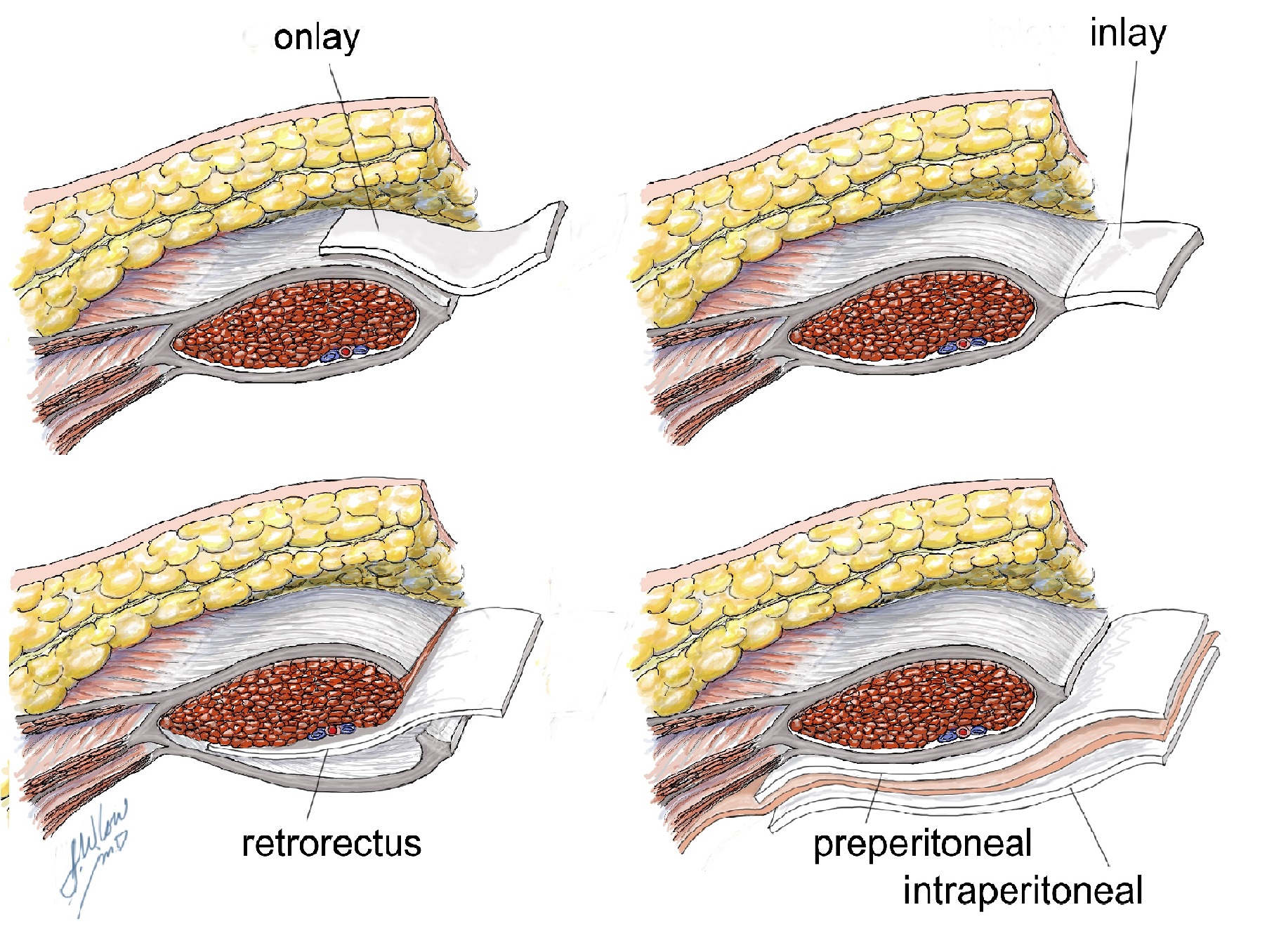 Table 2. Advantages and Drawbacks of Different Mesh Positions| Position | Advantages | Drawbacks | | Onlay | Simple; Fast; No visceral contact with mesh | More recurrence after repairs; Increased risk for seroma; Risks exposure and infection | | Sublay (Retrorectus or Preperitoneal) | Resistant to intra-abdominal pressure; Even distribution of tension; No cutaneous or visceral exposure | Technical challenge; Increased operative time | | Underlay | Resistant to intra-abdominal pressure; Even distribution of tension; No cutaneous exposure | Risk of bowel-related complications; Technical challenge | Table 3. Comparison of Mesh Materials| Mesh Type | Advantages | Drawbacks | | Synthetics | Cheap; Tensile strength; Composite barriers | Visceral Damage; Poor infection resistance; Complicates future procedures; Increased mesh pain | | Biologics | Increased infection resistance; Strong incorporation | Bulging; Decreased tensile strength; Cost | | Bioabsorbables | Handles like synthetics; Increased infection resistance; Early tensile strength; Resorbs after wound heals; Less likely to cause chronic pain | Lack of long-term data; Cost | CONCLUSIONS:There are clear indications for the use of PMA, with evident cost-utility and models for selecting high-risk patients, but treatment guidelines are lacking. Widespread adoption of PMA requires large scale pragmatic MCRCT research and CPT coding. Given the American Medical Association's recent approcal of a catagory III CPT code (0437T) to be implemented July 2016, the current outloook for PMA research in the US is positive. Beyond this, stakeholder collaboration is paramount for progress (Figure 2). The first step in breaking down the barriers preventing the use of PMA in a high-risk cohort of patients will be gaining awareness to build momentum for PMA adoption worldwide. 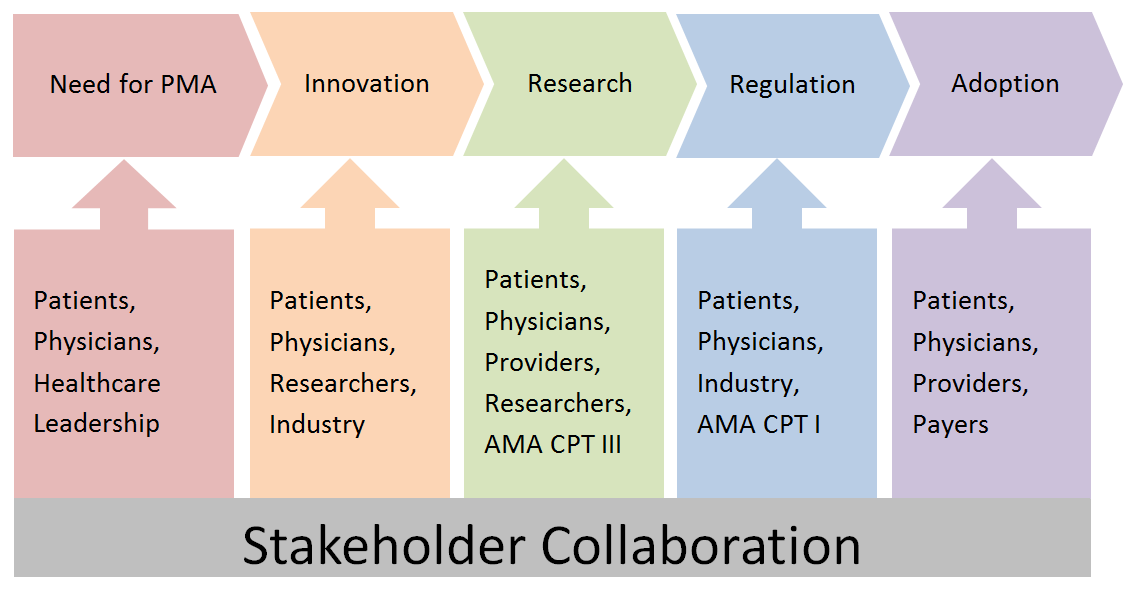
Back to 2016 Annual Meeting
|
|
