|
|
|
|
|
Back to 2016 Annual Meeting
Targeted Reinnervation for the Amputee, a Multi-Cohort Analysis
Corinne E. Wee, BA1, J. Byers Bowen, MD2, Jaclyn A. Kalik, BS1, Terry Zomerlei, MD2, Thuan V. Ly, MD3, Thomas J. Scharschmidt, MD3, Joel L. Mayerson, MD3, Raphael E. Pollock, MD, PhD4, Ian L. Valerio, MD2.
1Ohio State University College of Medicine, Columbus, OH, USA, 2Ohio State University Department of Plastic Surgery, Columbus, OH, USA, 3Ohio State University Department of Orthopaedic Surgery, Columbus, OH, USA, 4Ohio State University Department of Surgical Oncology, Columbus, OH, USA.
BACKGROUND: About 25% of major limb amputees will develop chronic localized symptomatic neuromas and phantom limb pain. A method to treat and possibly prevent these pain symptoms is Targeted Reinnervation (TR). TR is a surgical technique in which the native motor nerve of the target muscle is divided, and the amputated nerve is then transferred to the motor nerve, close to its entry point of the muscle. The resulting neurorrhaphy results in reduced pain symptoms and improved bio-prosthetic function. Prior studies by Dumanian et al have shown that chronic TR results in significant improvement in pain and increased prosthetic use. This study seeks to determine the success of TR at the time of amputation in preventing neuroma and phantom limb pain, as well as the success of TR in treating pre-existing neuroma and phantom limb pain.
METHODS: TR has been performed on sixteen patients at our institution. Fourteen of these patients underwent TR at the time of amputation; we refer to this as “primary TR.” Five patients underwent amputation due to oncologic disease, four patients for skeletal trauma, and five patients for chronic osteomyelitis. Two patients underwent TR secondary to painful neuroma following previous amputation. Adult subjects’ symptoms, satisfaction and functionality will be measured for one year by the Patient Report Outcomes Measurement Information System (PROMIS) questionnaire. One oncologic patient is 9 years old and will also be followed with the PROMIS questionnaire; however, this is not validated for subjects under 18 years old.
RESULTS: Follow-up data of greater than three months post-TR is available for nine patients. Two patients were lost to follow-up; one of these patients resumed follow-up after 3 months. Six patients have undergone TR recently and do not yet have adequate follow-up. All subjects have denied neuroma pain post-amputation. Majority of subjects initially reported phantom limb pain at their one-month follow-up, but all reported improvement by three months. The two patients whom underwent TR for treatment of symptomatic neuroma reported significant improvement in symptoms by two months.
CONCLUSIONS: Phantom limb and neuroma pain have been reported in amputee patients at three months post-operative at 9% and 2%, respectively. At three and six months post-operative from amputation and primary TR, all patients with sufficient follow-up reported no neuroma or phantom limb pain. Our early
data suggest that primary TR may aid in preventing painful neuroma and reducing phantom limb pain symptoms that are often problematic in residual limb patients/amputees. Additionally, primary TR may help alter the pain referral pathways from central to peripheral nervous system via earlier feedback and neural modulation leading to a greater improvement in pain and function, accelerated recovery, and improved quality of life. 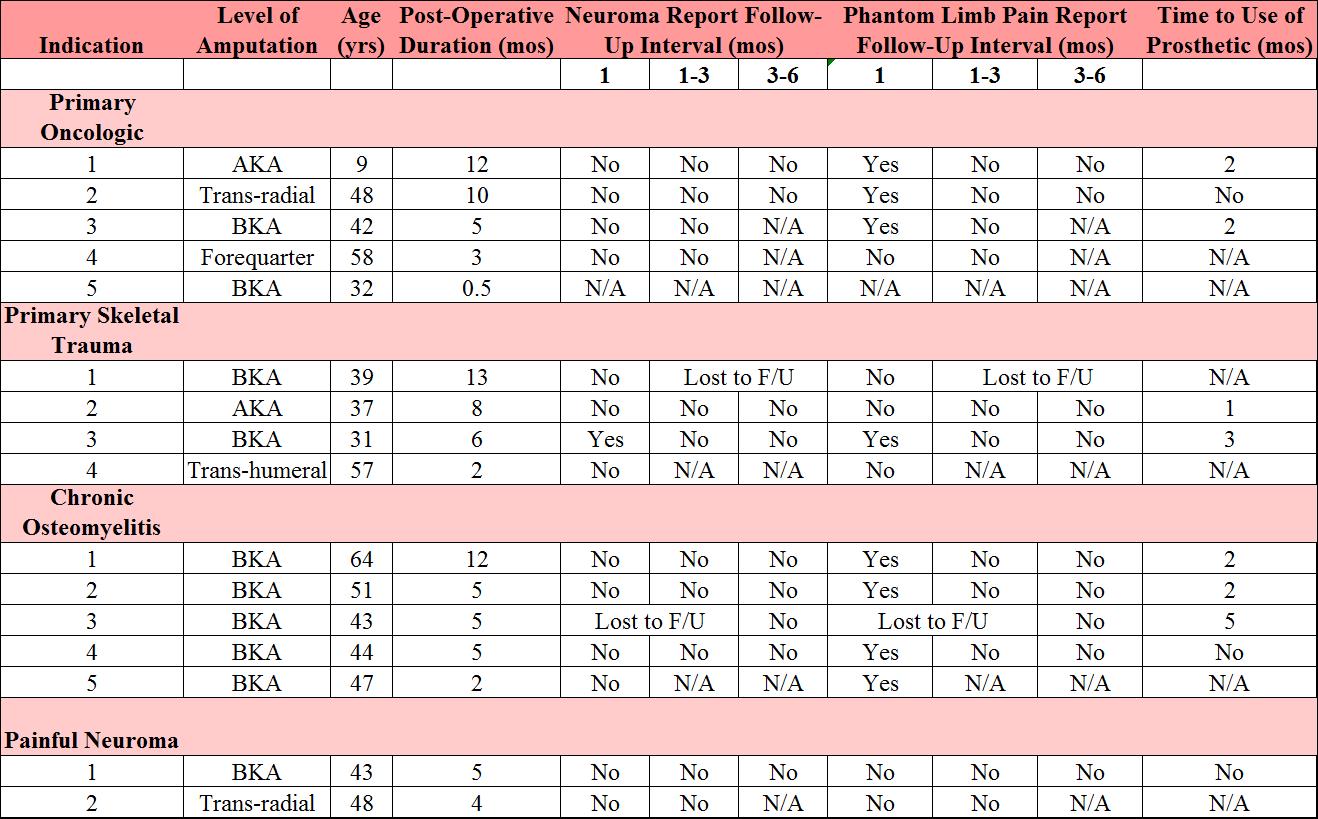
Back to 2016 Annual Meeting
|
|
