|
|
|
|
|
Back to 2016 Annual Meeting
Does Prophylactic Mesh Augmentation in Elective, Midline Laparotomy Reduce the Incidence of Incisional Hernia?
Sameer Shakir, MD1, Zachary Borab2, Michael Lanni1, Michael Tecce, DO1, John P. Fischer, MD1.
1University of Pennsylvania, Philadelphia, PA, USA, 2Drexel University College of Medicine, Philadelphia, PA, USA.
Background:
Surgery to correct incisional hernia (IH) affects 150,000 patients annually, with 1 in 3 repairs recurring within 9 years. Recent studies suggest preventing IH using prophylactic mesh augmentation (PMA) techniques, or reinforcing mesh at the index abdominal fascial closure, may be the solution to this hernia epidemic. We present a systematic review of PMA with the aim to highlight its efficacy in reducing the incidence of IH when compared to standard suture repair in high-risk patients.
Methods:
Adhering to PRISMA guidelines, a systematic review was performed of currently published randomized trials and prospective observational studies using PMA versus primary suture (PS) repair in elective, midline laparotomy at time of index abdominal fascial closure. Studies were assessed using the Cochrane Risk of Bias Tool. Primary endpoint was incidence of IH, assessed by meta-analysis. Secondary endpoints included postoperative complications, mesh type/location/fixation method, quality of life, and chronic pain.
Results:
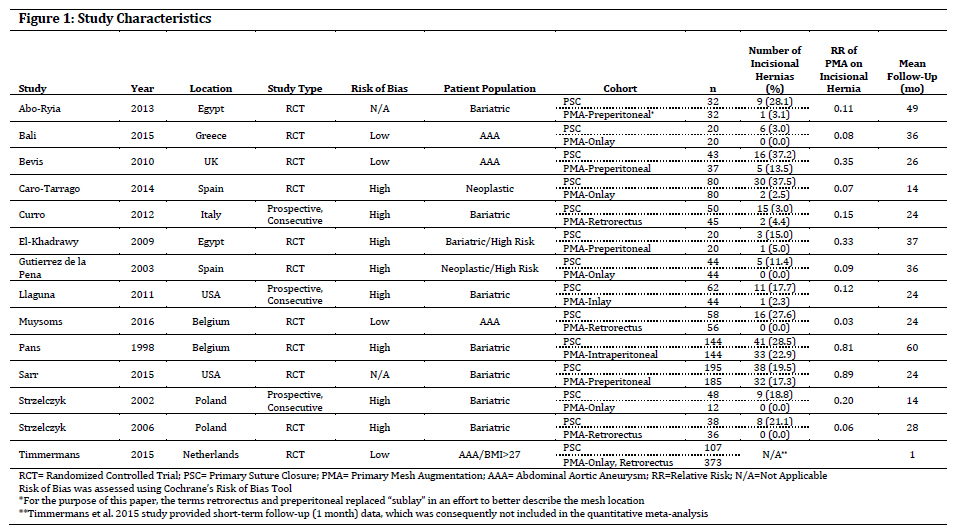
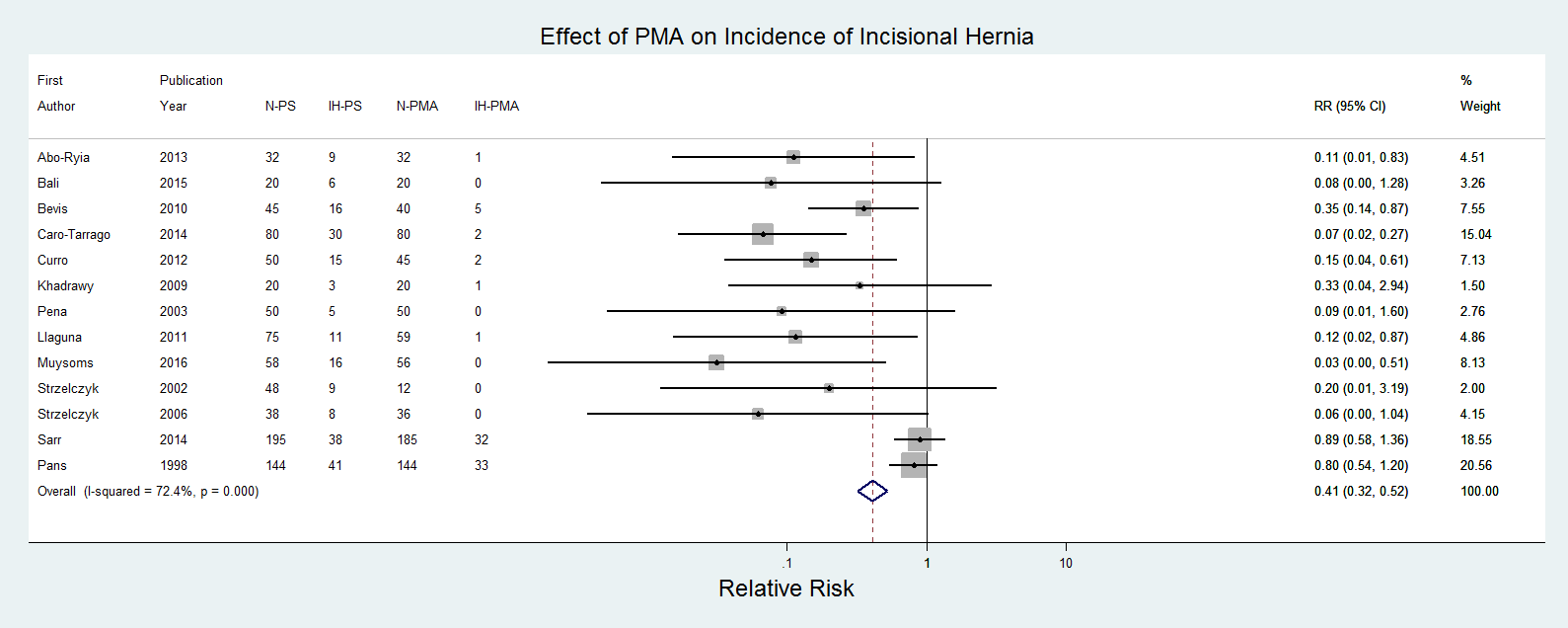
Fourteen studies [11 randomized controlled trials (RCTs) and three prospective trials] included 2114 patients, with 1152 receiving PMA. All studies included elective patients at high risk for postoperative IH due to the presence of abdominal aortic aneurysm (AAA), morbid obesity, and/or multiple comorbidities linked to IH. Four (28.5%) studies were at low risk of bias, 2 (14.3) unclear risk, and 8 (57.1) high risk. Weighted mean age of the studied populations was 50.04±14.16 years, 31.18±42.33% male, BMI 43.48±9.15, and length of follow-up (LOF) 25.61±14.35mos. There were no significant differences in age, gender, BMI, or LOF between groups. The weighted mean incidence of IH was 22.7±10.2% (mean ± STD) and 5.25±7.2% in the PS and PMA cohorts, respectively. PMA significantly decreased the risk of IH development, with Mantel–Haenszel (MH) pooled relative risk (RR) = 0.407 (95% CI 0.320 to 0.518; p<0.001). Weighted mean incidence of surgical site infections (SSI) did not significantly differ between groups (3.36±2.38% PS, 6.91±14.16% PMA; p<0.198), although mesh use was associated with an increased risk of developing postoperative seroma (3.42±2.71% PS, 9.08± 12.76% PMA) [MH pooled RR 2.121 (95% CI 1.496 to 3.008); p<0.001)]. Figures 1 and 2 provide table and graphical summaries of additional outcome measures.
Conclusions:
PMA is associated with a 60% postoperative IH risk reduction when compared to traditional suture repair for high-risk patients undergoing elective, midline laparotomy closure. Moreover, PMA appears to be safe and efficacious in the high-risk patient population, with current data revealing comparable postoperative complication profiles, barring a slightly increased rate of seroma. Despite this verification, PMA evidence from large domestic pragmatic trials is simply lacking. Widespread adoption of PMA and identifying evidence-based guidelines will greatly benefit from our institution’s introduction of a dedicated Category III CPT code (0437T) in July 2016 by the American Medical Association for prophylactic mesh augmentation.
Back to 2016 Annual Meeting
|
|
