Back to 2016 Annual Meeting
Histone Deacetylase Inhibitors Enhance Cytotoxicity Towards Breast Cancer While Preserving the Wound Healing Function of Adipose Derived Stem Cells
Kiavash R. Koko, MD, Shaohua Chang, PhD, Ashleigh L. Rapp, MD, Ryan S. Nolan, MD, Marc W. Fromer, MD, Spencer A. Brown, PhD, Martha S. Matthews, MD, Dorothy Bird, MD.
Cooper University Hospital, Camden, NJ, USA.
Introduction: Paclitaxel improves pathologic response of breast cancer resections; however, it may negatively affect the wound healing function of human adipose derived stem cells (hASC) and impair reconstructive surgery. Histone deacetylase inhibitors (HDACi) modify epigenetic regulation of gene expression. HDACi also stabilize microtubules similarly to Paclitaxel; therefore, combining these drugs creates a synergistic mechanism of cell cycle arrest. We aim to combine these drugs in order to enhance cytotoxicity towards breast cancer cells, while preserving the wound-healing function of hASCs for downstream reconstructive applications.
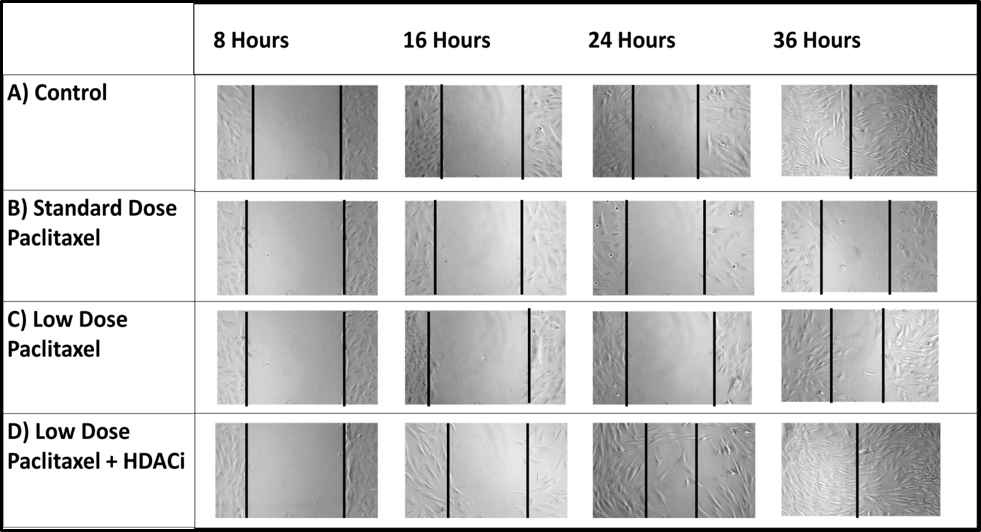
Methods: Triple negative breast cancer cells (MBA-MB-231) and hASCs (IRB approved clinical isolates) were treated with with a standard physiologic dose of Paclitaxel [1.0uM] or a low dose Paclitaxel [0.1uM] combined with the HDACi: Suberoylanilide Hydroxamic Acid (SAHA.) Cell viability was measured via MTT assay. Gene expression of hASCs was measured by quantitative real-time PCR. Functional wound healing was measured via cell migration in a standardized fibroblast scratch assay.
Results:
Cell Viability (%): Standard-Dose Paclitaxel [SP] vs Low-Dose Paclitaxel + SAHA [LP+S]
•
Breast Cancer Cells (n=9): [SP: 68% +/- 8.3] vs [LP+S: 60.8% +/- 6.6] p=0.31
•
Adipose Stem Cells (n=9): [SP: 76% +/- 7.1] vs [LP+S: 105.7% +/- 16.1] p<0.05
Gene Expression: fold change of pro-inflammatory genes IL-1b, IL-6, and the pro-apoptotic gene FAS decreased in the [LP+S] group vs [SP] group though not statistically significant.
•
IL-1b (n=5): [SP: 4.1 +/- 2.2] vs [LP+S: 2.1 +/- 0.8] p=0.27
•
IL-6 (n=5): [SP: 1.4 +/- 1.4] vs [LP+S: 0.7 +/- 0.3] p=0.52
•
FAS (n=5): [SP: 0.8 +/- 0.03] vs [LP+S: 0.7 +/- 0.1] p=0.53
Wound Healing: Dermal fibroblasts healed 24 hours sooner in the presence of hASCs treated with low-dose Paclitaxel + HDACi [LP+S] vs hASCs treated with standard-dose Paclitaxel [SP]:
•
Wound healing time: [SP: 48hrs] vs [LP+S: 24hrs]
Conclusion: Combining HDACi with low-dose Paclitaxel improved cytotoxicity towards breast cancer cells and decreased cytotoxicity towards hASC. Decreasing trends in inflammatory and apoptotic markers suggests enhanced wound healing ability as also underscored by improved healing in our dermal fibroblast scratch assay. These results indicate the addition of HDACi to existing chemotherapy regimens may potentially improve oncologic results as well as outcomes following reconstructive surgery.
Back to 2016 Annual Meeting
|
