|
|
|
|
|
Back to 2016 Annual Meeting
Clinical assessment one year after whole eye transplantation in a rodent
Lin He, M.D.1, Chiaki Komatsu, M.D.1, Yang Li, M.D.2, Maxine R. Miller, M.D.3, Yolandi Merwe, B.Eng3, Katie Lucy, B.S.3, Huamin Tang, M.D.1, Ian Rosner, B.S.1, Hongkun Wang, M.D.1, Mario G. Solari, M.D.1, Gadi Wollstein, M.D.3, Joel S. Schuman, M.D.4, Kevin C. Chan, Ph.D.5, Kia M. Washington, M.D.1.
1Department of Plastic Surgery, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA, 2Department of Plastic Surgery, Xijing Hospital, FMMU, Xi'an, China, 3Department of Ophthalmology, UPMC eye center, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA, 4Department of Ophthalmology, New York University Langone Medical Center, New York University School of Medicine, New York City, NY, USA, 5Department of Ophthalmology, UPMC Eye Center, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA.
Background: Approximately 39 million people worldwide suffer from blindness. Whole eye transplantation (WET) offers the opportunity to provide a viable optical system to recipients with irreversible vision loss. We have established an orthotopic vascularized whole eye transplant model in the rat. The purpose of our study is to evaluate gross morphology, structural integrity and aqueous humor dynamics in a long-term WET survivor, in particular to examine the changes over time in the native (contralateral) eye in the transplanted rat.
Methods: A syngeneic transplant was performed in a Lewis rat. The donor flap is composed of ocular tissue anterior to the optic chiasm, skin of the eyelid and external ear. The recipient site was prepared by removing a similar region of skin and ocular tissue with the optic nerve cut at the base of the globe. The graft was transplanted to the recipient and vascular anastomoses and the optic nerve coaptation were performed. Optical coherence tomography (OCT), gadolinium-enhanced magnetic resonance imaging (Gd-enhanced MRI) and electroretinography (ERG) were performed to evaluate the viability and structural integrity of the eyes of the long-term WET survivor and compared with a naïve, age-matched rat as a control.
Results: The long-term WET survivor and the naïve, age-matched control rat were more than 400 days old at time of OCT, MRI, and ERG analysis. Corneal opacification prohibited OCT imaging of the retina of the transplanted eye. OCT of the cornea and retina of the native (contralateral eye) corresponded with the naïve eyes of the control (age-matched) rat. Gd-enhanced MRI imaging revealed that aqueous humor dynamics in the native eye were comparable to eyes of the control rat. The native eye in the transplanted rat had a normal electrical response with electroretinogram (ERG), which was comparable to an age-matched control rat. Aqueous humor dynamics were compromised in the transplanted eye, and there was no evidence of electrical response with ERG analysis.
Conclusions: We have established a viable orthotopic model for vascularized whole eye transplantation in the rat. The structural integrity and function are relatively maintained in the native eye more than 400 days after whole eye transplantation and comparable to the age-matched control eyes. Thus there was no evidence of sympathetic opthalmia in the native (contralateral) eye of a long-term WET survivor. To our knowledge this is the world’s first report of long-term clinical assessment after whole eye transplantation.
Figures: Fig1: The frontal view of the long-term WET survivor; Fig 2: The OCT of the long-term WET survivor and age-matched control rat; Fig 3: The Gd-enhanced MRI at different time after Gd administration. 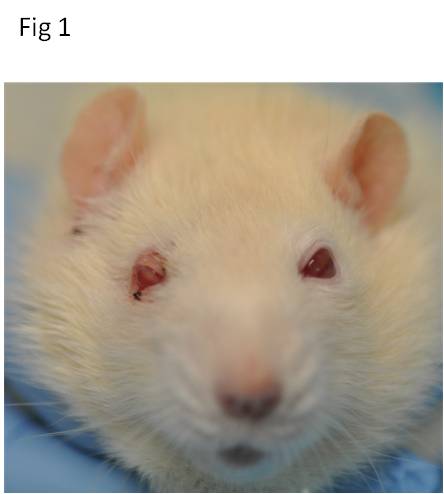 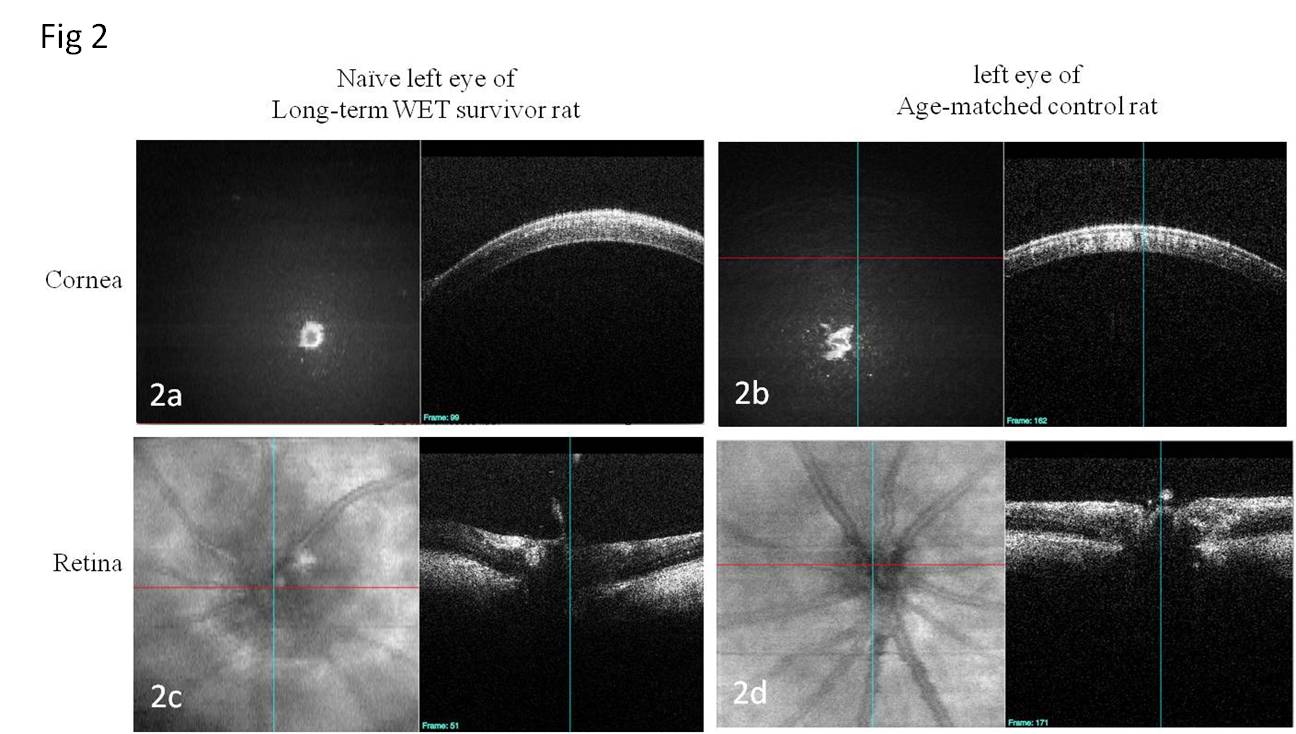 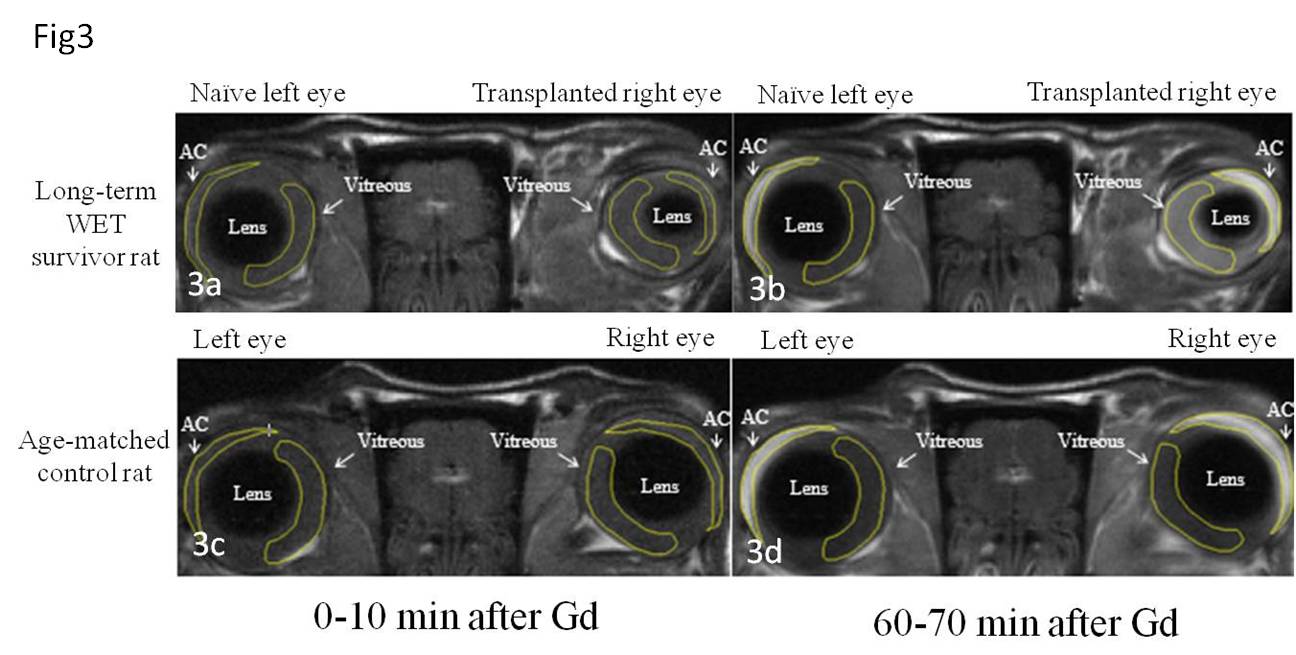
Back to 2016 Annual Meeting
|
|
