Back to 2016 Annual Meeting
Systematic Review of the Utilization of Clinical Decision Support Systems in Surgery
Zachary Borab, BA1, Michael Lanni2, Michael Tecce, DO2, John Fischer, MD2.
1Drexel University College of Medicine, Philadelphia, PA, USA, 2University of Pennsylvania Health System, Philadelphia, PA, USA.
BACKGROUND: The opportunity for risk reduction in the surgical setting includes the incorporation of shared decision making and informed consent. Computer based clinical decision support systems (CDSS) and risk models can bridge the knowledge gap that exists in predicting operative outcome. Several models are used in surgical fields but the evidence to evaluate their clinical relevance is scarce. CDSS can be used for prediction, but their use also extends to patient education, physician guideline adherence, and adverse event prevention. This systematic review summarizes the current scientific evidence for using clinical decision support tools in surgery and identifies areas of implementation in plastic surgery.
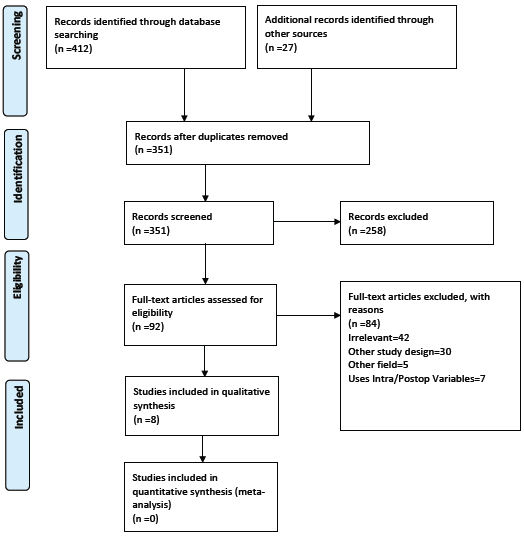
METHODS: A systematic review of was performed by a thorough search of 10 terms using PubMed, MEDLINE, Embase, Scopus, and Cochrane databases in April 2016. This resulted in 324 individual articles subject to inclusion and exclusion criteria.
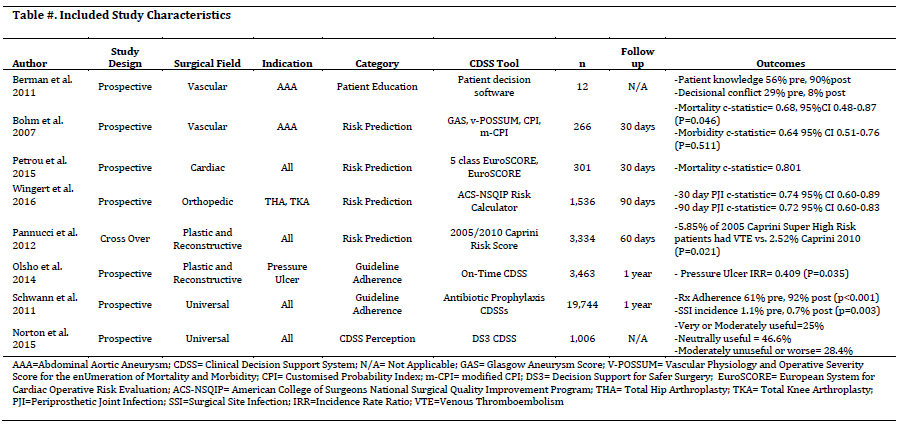
RESULTS: A total of 8 articles met inclusion criteria, 7 from the literature search and 1 from a manual reference search. These articles evaluated the implementation of different CDSS in surgery and allied services. This review categorized the articles by four study purposes: patient education, risk prediction, guideline adherence, and user perception. One article used CDSS to educate patients prior to AAA surgery and effectively reduced their decisional conflict 29% to 8%. Four articles tested the preoperative risk prediction in different CDSS risk models. One was found to have good measure (c-statistic>0.8) in discriminating postoperative complications and two had only a fair measure (c-statistic>0.7). Another study compared Caprini 2005 and 2010 risk models to predict venous thromboembolism in plastic surgery patients. The 2005 Caprini score more accurately predicted 60 day postoperative VTE. CDSS and guideline adherence was prospectively tested in the administration of perioperative antibiotics and in pressure ulcer prevention. Antibiotic prophylaxis increased from 61%-92% (p<0.001) with CDSS and surgical site infection was reduced from 1.1% to 0.7% (p=0.003). Pressure ulcers incidence rate ratio was 0.409 (p=0.035) after CDSS implementation. The last article measured surgeon perception of CDSS that provided preoperative risk assessments at the patient level. The tool was found to be neutral in 45% of users and very or moderately useful by 25% of users.
CONCLUSIONS: Further large prospective studies are needed to validate clinical usefulness of CDSS. The tool should be user friendly and promptly provide useful information that can then be used to make informed decisions. Future models should integrate surgical risk patient data from electronic health records to create an efficient computerized clinical decision support system. Of the models that are available today, it appears that most can be used to estimate preoperative risk with at least a fair to good measure in discrimination.
Back to 2016 Annual Meeting
|
