|
|
|
|
|
Back to 2016 Annual Meeting
A Risk Model and Cost Analysis of Postoperative Incisional Hernia Following 4,608 Open Hysterectomies—Defining Indications and Opportunities for Risk Reduction
Michael G. Tecce, DO1, Marten N. Basta, MD2, Valeriy Shubinets, MD1, Michael A. Lanni, BS1, Michael N. Mirzabeigi, MD1, Laura Cooney, MD1, Suneeta Senapetti, MD, MSCE1, Ashley F. Haggerty, MD1, Stephen J. Kovach, MD1, John P. Fischer, MD1.
1University of Pennsylvania, Philadelphia, PA, USA, 2Brown University, Providence, RI, USA.
BACKGROUND: Incisional hernia (IH) is a major complication following open abdominal hysterectomy. The purpose of this study is threefold: (1) to assess the incidence and health care cost of surgically repaired IH after open abdominal hysterectomy; (2) identify actionable, perioperative risk factors; and (3) create a predictive risk model.
METHODS: We conducted a retrospective review of patients who underwent hysterectomy through an open abdominal approach between 1/2005 and 6/2013 within the University of Pennsylvania Health System. The primary outcome of interest was post-hysterectomy IH. Univariate and multivariate cox proportional hazard analyses were performed to identify perioperative risk factors. Patients with prior hernia, less than 1 year follow-up, or emergency surgeries were excluded. Cox hazard regression modeling with bootstrapped validation, risk factor stratification, and assessment of model performance was performed.
RESULTS: A total of 4,608 patients underwent open abdominal hysterectomy during the study period. Eighty-four patients (1.82%) required IH repair and generated significantly higher costs of care ($68,077 vs. $22,107, p<0.001) (Table 1). Ten risk factors were identified and included in the final adjusted risk model, the strongest of which were acute intraabdominal inflammatory process (HR=3.75 [1.46 9.63]) and liver disease (HR=2.61 [1.554.40]). Extreme risk patients experienced the highest incidence of surgically repaired IH after hysterectomy (21.7%), followed by the high risk group (7.3%), moderate risk group (2.3%), and low risk group (0.6%) (C-statistic= 0.81) (Figures 1 and 2).
Table 1. Summary of Risk-Stratification and Secondary Outcomes| Risk Group (Score Range) | Total - N(%) | Hernia - N(%) | Reoperation - N(%) | LOS - Ave. (SD) | Days to Readmit - Ave.(SD) | Readmit Cost - Ave.(SD) | Combined Cost - Ave.(SD) | | Low (0 to 1) | 2,929 (63.6%) | 19 (0.6%) | 602 (20.6%) | 3.2 (2.4) | 423 (566) | $13,920 (30,112) | $16,521 (20,220) | | Moderate (2 to 4) | 1,278 (27.7%) | 29 (2.3%) | 393 (30.8%) | 4.6 (4.7) | 298 (485) | $24,870 (41,501) | $27,810 (34,245) | | High (5 to 6) | 355 (7.7%) | 26 (2.3%) | 158 (44.5%) | 6.9 (8.0) | 267 (429) | $43,730 (58,056) | $51,383 (59,520) | | Extreme (7 and up) | 46 (1.0%) | 10 (21.7%) | 30 (65.2%) | 7.7 (5.5) | 208 (295) | $67,430 (79,583) | $78,233 (77,889) | | Total: | 4,608 (100%) | 84 (1.8%) | 1,183 (25.7%) | 3.9 (4.0) | 358 (524) | $22,514 (42,551) | $22,955 (33,030) | 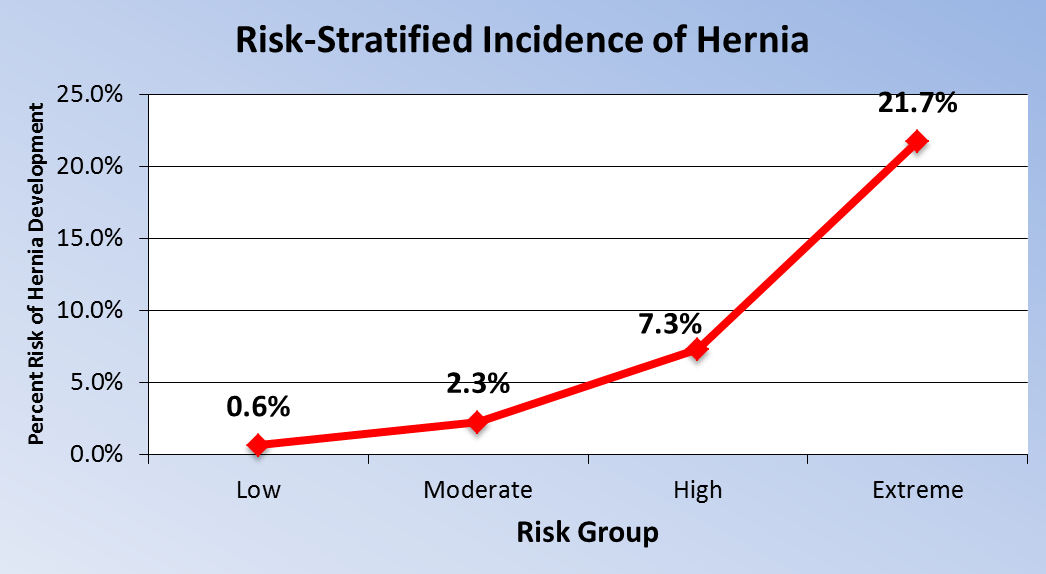  CONCLUSIONS: CONCLUSIONS:This study identifies perioperative risk factors for IH and provides a risk prediction instrument (Figure 3) to accurately stratify patients, augment preoperative counseling, and potentially imply risk reduction techniques. 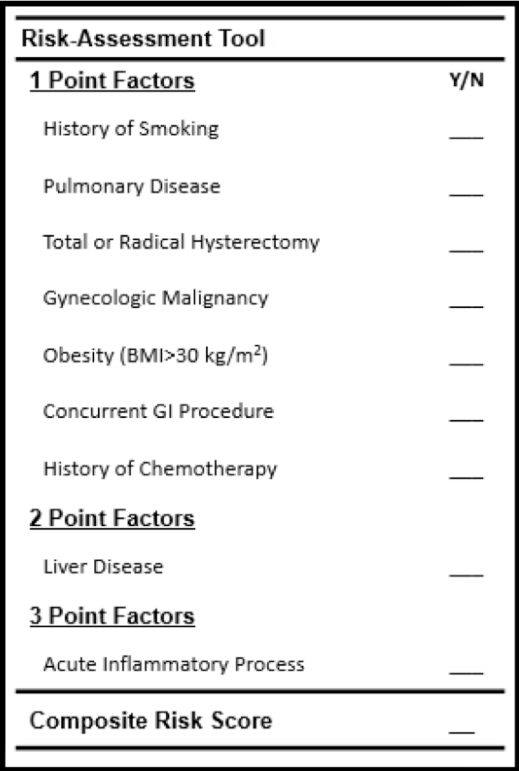
Back to 2016 Annual Meeting
|
|
