Back to 2016 Annual Meeting
The Effect of Neoadjuvant Chemotherapy Compared to Adjuvant Chemotherapy in Healing after Nipple-Sparing Mastectomy
Jordan D. Frey, MD, Mihye Choi, MD, Nolan S. Karp, MD.
NYU Langone Medical Center, New York, NY, USA.
BACKGROUND: Nipple-sparing mastectomy (NSM) is the latest advancement in the surgical treatment of breast cancer. As indications continue to expand, patients with more advanced disease are undergoing NSM. Data regarding the effects of chemotherapy on NSM remains scarce. We therefore aim to investigate the effects of neoadjuvant and adjuvant chemotherapy on reconstructive outcomes in NSM to allow for improved risk stratification in this patient population.
METHODS: All patients undergoing nipple-sparing mastectomy at New York University Langone Medical Center from 2006 to June 2015 were identified with institutional review board approval. Results were then stratified by patients who had and had not received neoadjuvant or adjuvant chemotherapy.
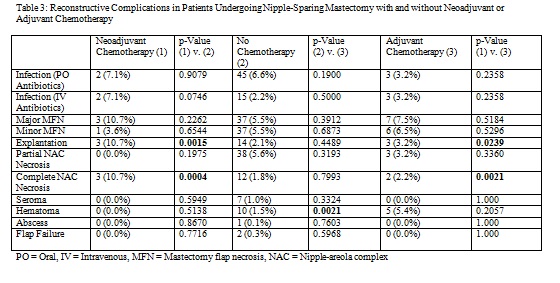
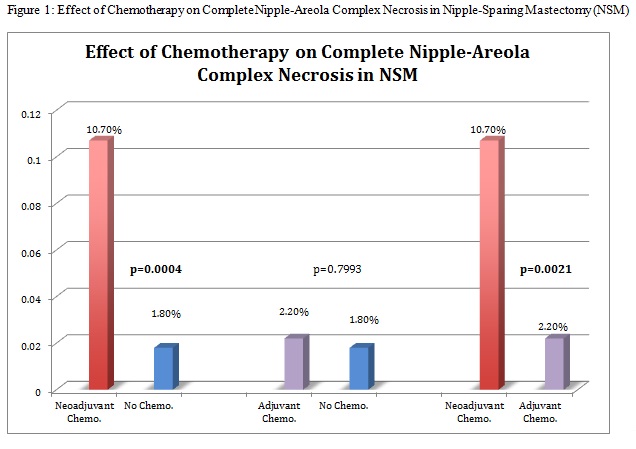
RESULTS: A total of 845 nipple-sparing mastectomies (NSM) were performed during the study period. Of these, 28 NSMs were performed in those who received neoadjuvant chemotherapy while 93 were performed in patients who received adjuvant chemotherapy. Compared to those with no chemotherapy, NSMs who received neoadjuvant chemotherapy were significantly more likely to have implant explantation (p=0.0015) and complete nipple-areola complex necrosis (p=0.0004). Complications were otherwise equivalent between the two groups. Compared to NSMs in patients with no chemotherapy, those in patients who received adjuvant chemotherapy were significantly more likely to have a hematoma (p=0.0021). Complications were otherwise equivalent between these two groups. NSMs in patients who received neoadjuvant chemotherapy were compared to those in patients who received adjuvant chemotherapy. Those who received neoadjuvant chemotherapy were significantly more likely to have explantation (p=0.0239) and complete nipple-areola complex necrosis (p=0.0021). A subset of NSMs in patients who received both neoadjuvant and adjuvant chemotherapy was compared to those who received neoadjuvant chemotherapy only. Those who received both neoadjuvant and adjuvant chemotherapy were significantly more likely to have complete nipple-areola complex necrosis (p<0.0001).
CONCLUSIONS: Overall, NSM is safe to perform in the setting of neoadjuvant and adjuvant chemotherapy. However, neoadjuvant chemotherapy significantly increases risk of wound healing complications compared to patients with no chemotherapy; a trend that is not observed with adjuvant chemotherapy. A synergistic effect between neoadjuvant and adjuvant chemotherapy with regards to reconstructive complications is also noted. This is the first such study to comparatively examine the impact of neoadjuvant and adjuvant chemotherapy on reconstructive outcomes in NSM.
Back to 2016 Annual Meeting
|
