|
|
|
|
|
Back to 2016 Annual Meeting
Transversus Abdominis Plane Blocks with Single-Dose Liposomal Bupivacaine Reduce Length of Stay Following Abdominally-Based Microsurgical Breast Reconstruction
Julie N. Kim, MD1, Eric M. Jablonka, MD2, Andreas M. Lamelas, MD2, Tomer Avraham, MD1, Nathan Molina, BA3, Bianca Molina, MD1, Joseph H. Dayan, MD4, Mark L. Smith, MD, FACS1.
1Division of Plastic Surgery, Mount Sinai Beth Israel, New York, NY, USA, 2Division of Plastic and Reconstructive Surgery, Mount Sinai Hospital, New York, NY, USA, 3UC Irvine College of Medicine, Irvine, CA, USA, 4Memorial Sloan Kettering Cancer Center, New York, NY, USA.
Background
Microsurgical abdominally-based breast reconstruction (MABR) typically entails an inpatient length of stay between three to five days. In this study, we examined the effect of bilateral single-dose TAP nerve blockade using liposomal bupivacaine (BTBLB) on length of stay after MABR to see if it facilitated safe discharge by post-operative day two.
Methods
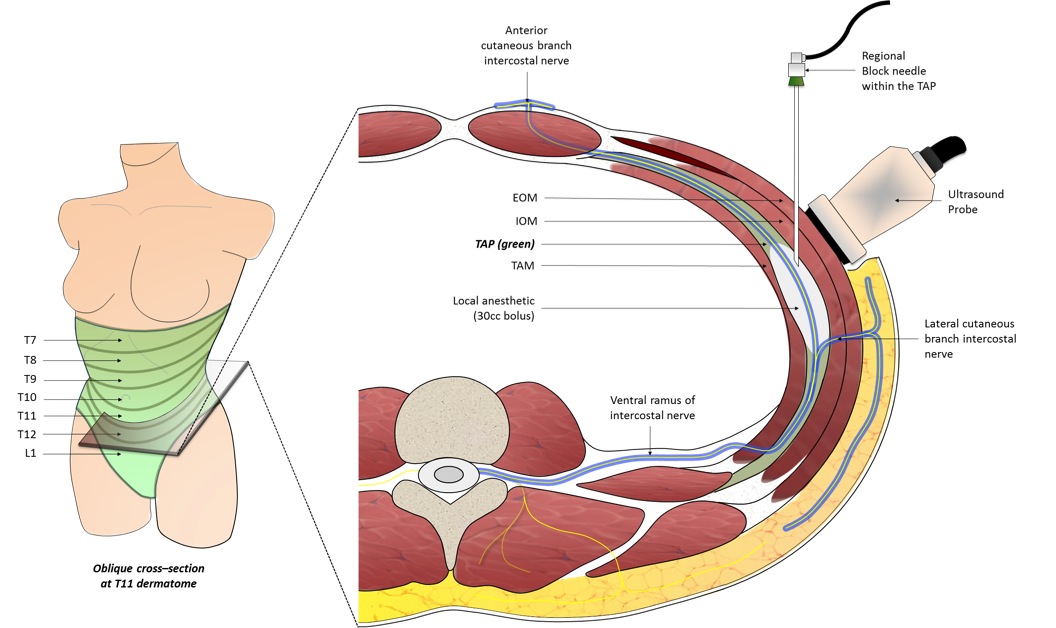
A single-center, single-surgeon (M.L.S.) retrospective analysis of patients undergoing MABR between 2010 and 2015 was performed. Ultrasound-guided trans-fascial injections were performed intra-operatively by the operating surgeon using a mixture of 20cc of 1.3% liposomal bupivacaine, 30cc of 0.25% of bupivacaine and 80cc of saline. A total of 30cc was injected per side into the transversus abdominis plane. A non-narcotic pain control regimen was used post-operatively and supplemented with narcotic analgesics as needed. Demographic factors, length of stay, inpatient opioid consumption and complications were reviewed and compared.
Results
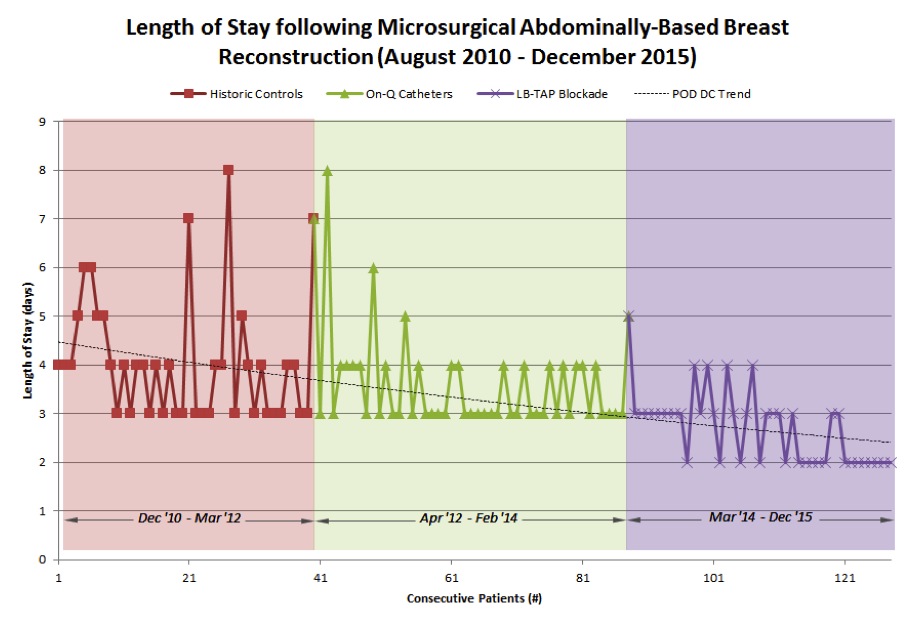
Between December 2010 and December 2015, 128 consecutive patients underwent a total of 182 abdominally-based free flaps. Of the 128 patients, 40 (62 flaps) patients received BTBLB, 48 (66 flaps) received continuous bupivacaine infusion TAP-catheters (CBITC), and 40 (54 flaps) received no locoregional analgesia. Patients who received BTBLB required significantly less narcotics during the first 48 hours (1st 24hrs: 6.6+-7.2mg vs 54.6+-52.0mg, p<0.0001, and 2nd 24hrs: 8.3+-8.3mg vs 34.8+-44.6mg, p=0.02) and had a significantly shorter hospital stay compared to historic controls (2.65+-0.66 days vs. 4.05+-1.26 days, p<0.0001) with most BTBLB patients (n=16, 67%) leaving on post-operative day two during the final study year. The CBITC group had a higher transfusion rate compared to BTBLB and historic control groups. There was no other significant difference in major complication rates or flap loss rates between the three groups.
Conclusion
MABR is the most common form of autologous reconstruction. The introduction of singe-dose liposomal bupivacaine to our practice in early 2014 allowed us to provide long-term analgesia to the abdominal donor site without the need for TAP-catheters and cumbersome external infusion pumps. Many institutions feel that POD 4 is the most appropriate day for discharge, as this gives adequate time for close flap observation and medical management. However, free flap take-back and salvage rates both drop significantly after 48 hours. Therefore, the incremental hospital costs for each flap that might be salvaged rise dramatically after the second post-operative day. Moreover, most payors only reimburse for the first two hospital days after routine mastectomy regardless of the breast reconstruction method.
TAP-blockade with long-acting liposomal bupivacaine performed during microsurgical abdominally-based breast reconstruction facilitates early patient discharge by post-operative day two without increased complications or rates of flap loss.
Back to 2016 Annual Meeting
|
|
