Back to 2016 Annual Meeting
The Use of Antibiotic Beads Following Breast Implant Infection to Forgo IV Antibiotics and Salvage the Implant
Rami D. Sherif, BA, Michael Ingargiola, MD, Philip J. Torina, MD, Marco A. Harmaty, MD.
Icahn School of Medicine at Mount Sinai, New York, NY, USA.
Background: Immediate breast reconstruction (IBR) is often deferred in the setting of postmastectomy radiotherapy (PMRT) due to increased complication rates; however, patients and physicians are increasingly aware of improved health related quality of life associated with reconstruction so may be accepting of tradeoffs. No national study has measured utilization of IBR in patients undergoing PMRT compared to a control group. Such information is imperative for understanding practice patterns at a broader level and for creating an ideal reconstruction algorithm for radiated patients. The study aim is to analyze trends in rates and methods of IBR in the setting of PMRT using the National Cancer Data Base (NCDB). The hypothesis is that radiation is a diminishing relative contraindication to IBR.
Methods: NCDB was queried from 2004 to 2013 for women that underwent mastectomy with and without IBR. Socio-demographic and oncological covariates were tabulated. Patients were divided into groups based upon whether or not they received PMRT. Trend analyses were done for rate and method of IBR using poisson regression to determine incidence rate ratios (IRR). Logistic regression was used to calculate the odds of undergoing IBR with PMRT after adjusting for covariates.
Results: The increase in rate of IBR was greater in radiated compared to non-radiated patients (IRR: 1.12 versus 1.09). After adjusting for covariates, radiated patients were significantly less likely to receive breast reconstruction (Odds Ratio: 0.70). Rates of implant and autologous reconstruction increased significantly from 2004 to 2013 (Fig. 1 and 2). For both methods, the rate increase was significantly greater in those receiving PMRT compared to non-radiated patients (implants: IRR 1.15 versus 1.11 and autologous: IRR 1.08 versus 1.06 respectively). In 2004 and 2005 autologous methods were the preferred reconstructive technique in the setting of PMRT (p<0.05). Thereafter, PMRT was not associated with a specific reconstructive method.
Conclusions: IBR rates are increasing in the US in both radiated as well as non-radiated patients, but to a greater extent in radiated patients. PMRT remains a perceived relative contraindication albeit to a lesser degree over time. The method of IBR performed in the setting of PMRT did not differ significantly after 2005. Implants have surpassed autologous tissue as the most common method of reconstruction both in radiated and non-radiated patients. 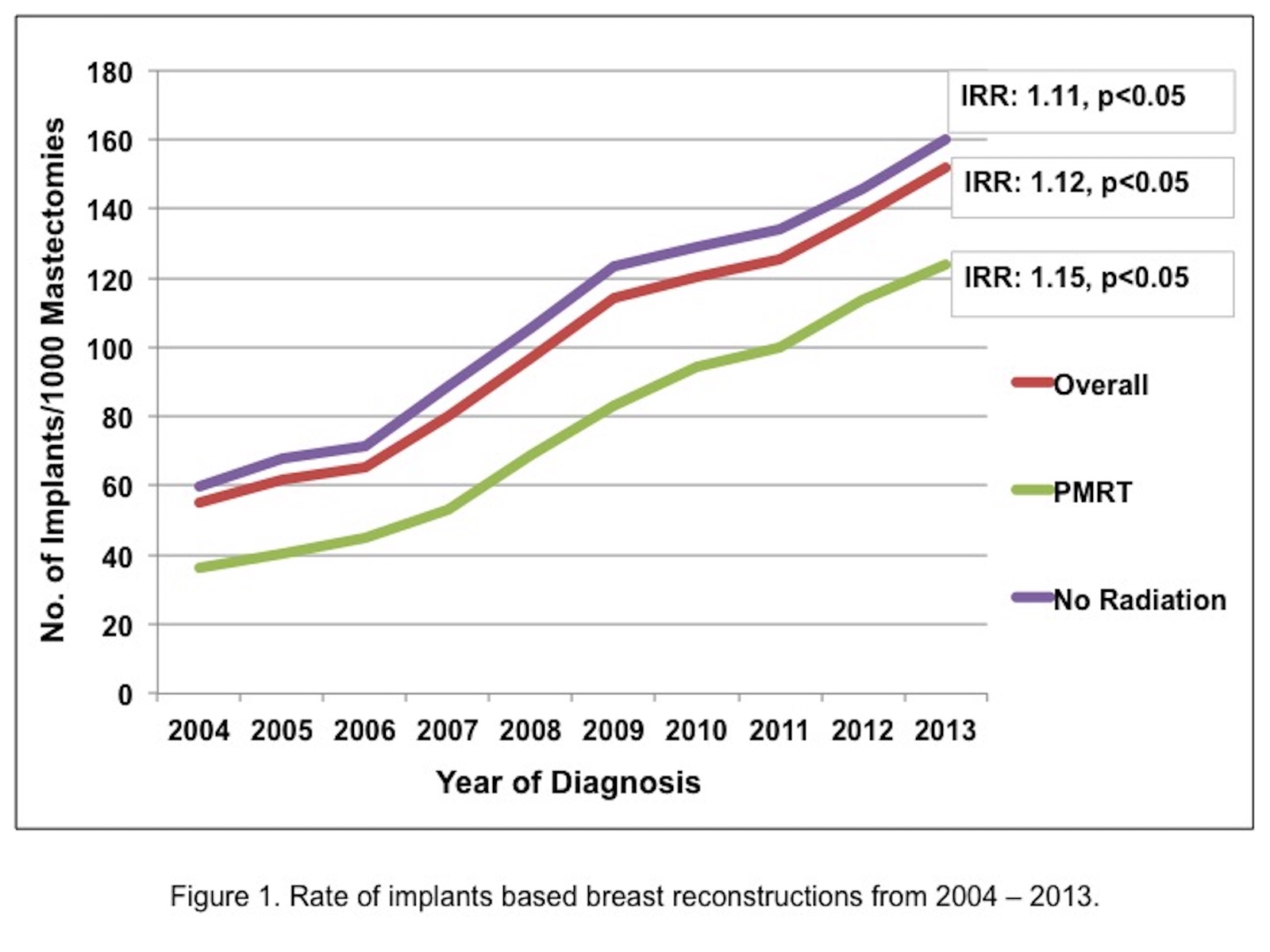 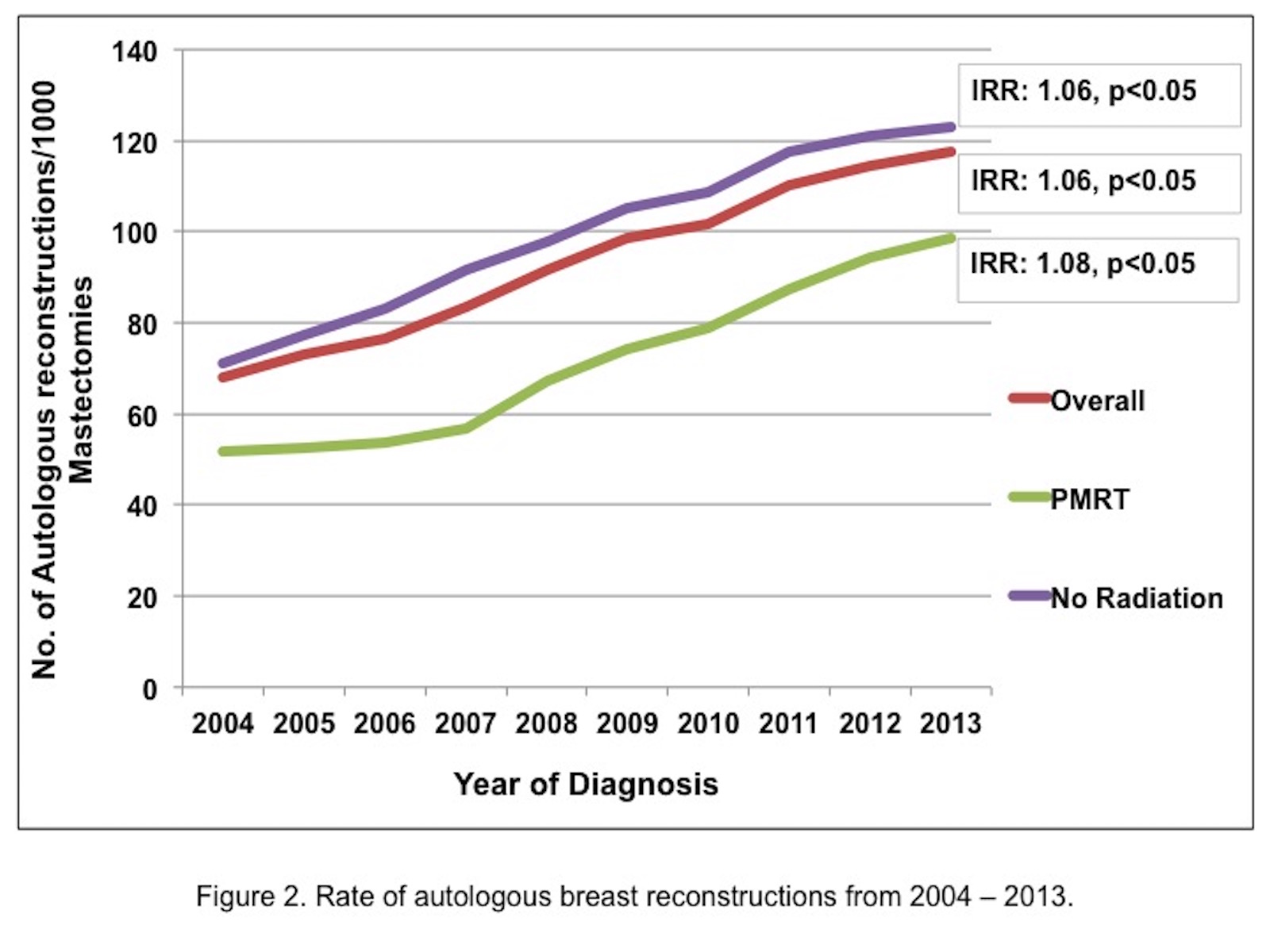
Back to 2016 Annual Meeting
|
