|
|
|
|
|
Back to 2016 Annual Meeting
A Validated Multi-Institutional Approach To Optimizing Outcomes Of Reduction Mammoplasty: A Critical Analysis Of 7,068 Patients
Pablo A. Baltodano, MD1, M. Eliann Reinhardt, B.S., B.M.2, Ashar Ata, PhD1, Usamah F. Simjee, B.S.1, Malcolm Roth, MD1, Ashit Patel, MBChB1.
1Albany Medical Center, Albany, NY, USA, 2Johns Hopkins University, Baltimore, MD, USA.
Background: Recent evidence suggest that compared to other elective non-reconstructive breast surgeries, reduction mammoplasty remains associated with significantly higher rates of overall morbidity, superficial surgical site infections, and wound disruptions (p< 0.05). We aimed to develop a validated risk model to identify patients at higher risk for postoperative surgical site morbidity (SSM) after reduction mammoplasty.
Methods: Retrospective review of all females undergoing reduction mammoplasties from the ACS-NSQIP 2005-2012 data. SSM included surgical site infection (SSI) and wound disruption events. Stepwise multivariable logistic regression was used to identify the risk factors associated with SSM. The model was validated using bootstrap replications (n=100) and Hosmer-Lemeshow test. The model was converted into a clinical risk score (CRS) predictive of SSM.
Results: We identified 7,068 reduction mammoplasties. Rate of 30-day SSM was 3.98%. Independent risk factors included resident participation(OR=1.5,95%CI:1.1-2.0,p=0.004), BMI(for every 5 unit increase: OR=1.3,95%CI:1.1-1.4,p<0.001), smoking(OR=1.6,95%CI:1.1-2.4,p=0.014), steroid use(OR=3.5,95%CI:1.4-8.4,p=0.006), and operation in 3rd quarter of the year(OR=1.5,95%CI:1.1-1.9,p=0.014). The factors were integrated into a CRS ranging from 0-16 (Table1). Predicted probability of SSM associated with each risk score was estimated (Table2). Predicted and observed risks of SSM were highly comparable (Figure1).
Conclusion: We present a validated risk stratification tool for predicting 30-day SSM following reduction mammoplasty using data that are readily available to the clinician. This may allow targeted screening and intervention in high-risk patients, better counseling, selective resident participation, and ultimately decrease overall health-care costs. This is the first study to date that provides a well-defined risk assessment tool to improve outcomes in reduction mammoplasty patients. Future studies should determine if implementation of our SSM risk score optimizes safety and reduces morbidity rates after reduction mammoplasty. 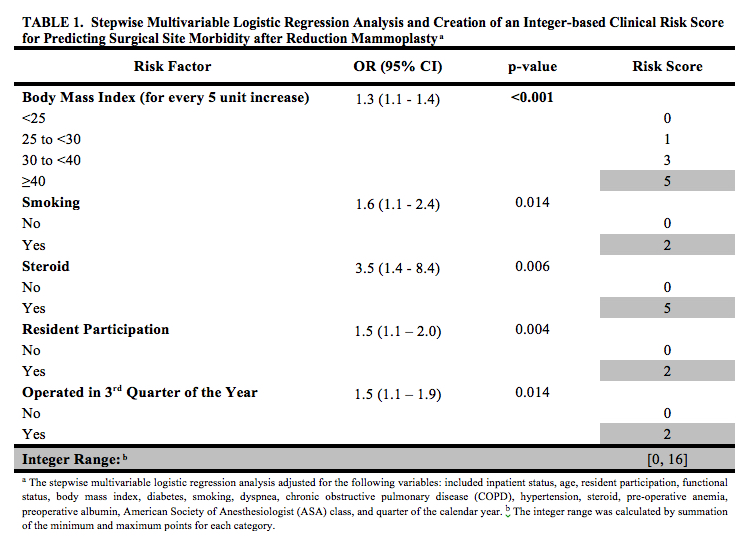 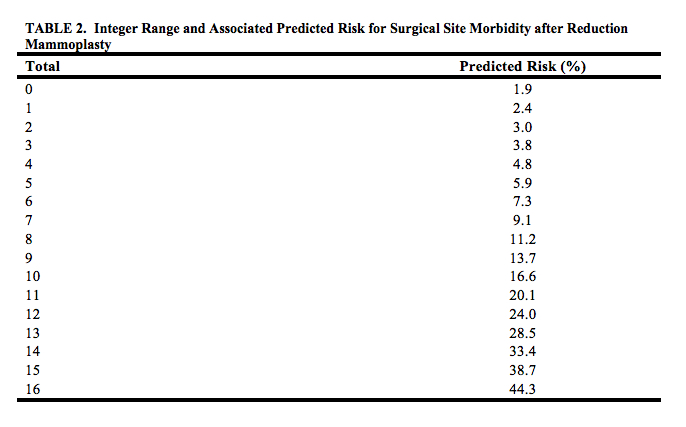 
Back to 2016 Annual Meeting
|
|
