|
|
|
|
|
Back to 2016 Annual Meeting
Timing of Cranial Vault Remodeling in Non-Syndromic Craniosynostosis: A Single Institution’s Thirty-year Experience
Joseph Lopez, MD MBA1, Alan Utria, BA1, Regina Cho, BA1, Gerhard S. Mundinger, MD1, George I. Jallo, MD1, Edward S. Ahn, MD1, Craig Vander Kolk, MD2, Amir H. Dorafshar, MBBS1.
1Johns Hopkins Hospital, Baltimore, MD, USA, 2Mercy Medical Center, Baltimore, MD, USA.
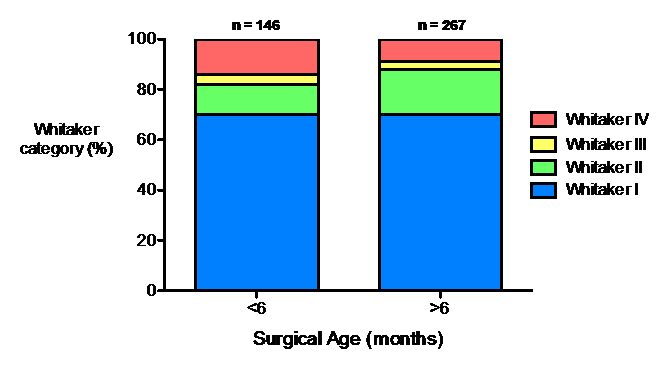
BACKGROUND: Due to the changing properties of the infant skull there is still no clear consensus on the ideal time to surgically intervene in cases of non-syndromic craniosynostosis (NSC). This study aims to shed light on how age at time of surgery may affect surgical outcomes and the subsequent need for reoperation. We hypothesized that age would not impact surgical outcomes as measured by Whitaker scores.
METHODS: A retrospective cohort review was conducted for patients with NSC who underwent primary cranial vault remodeling from 1990-2013. Patient demographics, characteristics, and surgical interventions were recorded. Postoperative outcomes were assessed by assigning each procedure to a Whitaker category. Multivariate logistic regression analysis was performed to determine the relationship between age at surgery and need for minor (Whitaker I/II) versus major (Whitaker III/IV) reoperation. Odds ratios (OR) for Whitaker category by age at surgery were assigned.
RESULTS: A total of 413 unique patients underwent cranial vault remodeling procedures for NSC during the study period. Average follow up was 5 years (SD 4 years). Demographically, the patient population consisted of 256 (62%) males, 339 (82%) Caucasians, 52 (13%) African Americans, and 8 (2%) Hispanics. Cranial vault remodeling procedures were categorized as anterior (175, 42%), posterior (90, 22%), subtotal (37, 9%), and multiple strip craniectomies (107, 26%). One hundred and forty six (35%) patients under the age of 6 months underwent cranial vault remodeling, compared to 267 (65%) patients greater than 6 months of age. There were 289 (70%) procedures that were classified as Whitaker category I, 65 (16%) procedures as category II, 13 (3%) procedures as category III, and 46 (11%) procedures as category IV. Multivariate logistic regression demonstrated increased odds of requiring major surgical revisions (Whitaker III/IV) in patients less than 6 months of age (OR=2.49, 95% CI: 1.05-5.93), and increased odds of requiring minimal surgical revisions (Whitaker I/II) in patients greater than 6 months of age (OR=2.72, 95% CI: 1.16-6.41).
CONCLUSIONS: Timing, as a proxy for the changing properties of the infant skull, is an important factor to consider when planning vault reconstruction in non-syndromic craniosynostosis. Our data demonstrates that patients operated on before 6 months of age had an increased odds ratio of requiring major surgical revisions. Furthermore, patients operated on after 6 months of age were more likely to require only minor revisions.
Back to 2016 Annual Meeting
|
|
