Back to 2016 Annual Meeting
Hyperbaric Oxygen Induces Healing by Improving Wound Microvasculature
Sarah C. Sorice, MD, Torbjörn Lundh, PhD, Alexander Li, BS, Kristine Rustad, MD, Venita Chandra, MD, Jeanie Parsley, PT, Robert Robertson, RN, Subhro Sen, MD, Geoffrey C. Gurtner, MD.
Stanford University, Palo Alto, CA, USA.
Background: The efficacy of hyperbaric oxygen therapy (HBOT) to facilitate wound healing in diabetic lower extremity ulcers is well established. The impact of HBOT however, on tissue perfusion and flow is not known. The purpose of this pilot study was to ascertain the effects of HBOT on the microvasculature of chronic wounds as assessed by fluorescent angiography.
Methods: Patients underwent fluorescent angiography at 6 different time points: immediately prior and immediately after the first, second and 20th HBOT treatments. Photo imaging with infrared camera began concurrently with the initiation of the IC- Green™ injection and lasted for 2.5 minutes. All videos were analyzed via MATLAB. The wound bed and the peri-wound area were then outlined as masks for the image analysis. The 1st and 2nd derivative were subsequently taken to define several time points of interest.
Results: Immediately after HBOT, there was evidence of increased flow. The onset of arterial inflow and venous outflow occurred increasingly earlier in response to consecutive HBOTs indicating an HBO mediated vasodilitory effect. In addition, the time interval between the onset of arterial inflow and venous outflow was longer in response to cumulative treatments of HBOT, suggesting increased overall time in the capillary bed. After prolonged treatments with HBOT (20 treatments), both onset of arterial inflow and venous outflow occurred significantly later compared to baseline and the initial two HBO treatments potentially indicating vascular redistribution via neo- angiogenesis. This correlated well with decreasing wound size.
Conclusion: This pilot study demonstrates that hyperbaric oxygen therapy appears to immediately impact the microcirculation both on an inflow (arterial) and outflow (venous) level. Long term HBOT appears to affect the architecture of the peri-wound microvasculature by inducing capillary neo-angiogenesis. These results offer an insight into the potential mechanism of HBOT and may direct future applications. 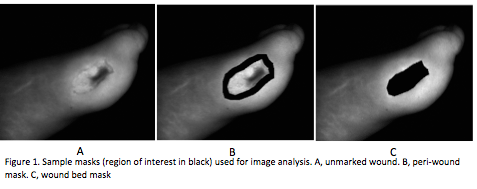 
Back to 2016 Annual Meeting
|
