|
|
|
|
|
Back to 2016 Annual Meeting
Single Institutional Experience with 12,165 Median Sternotomies: A Simple Risk Assessment Tool for Deep Wound Infection
Michael G. Tecce, DO, Alejandro Conejero, MD, Michael A. Lanni, BS, Ari M. Wes, BA, Jeffery I. Rohrbach, MSN, Joseph M. Serletti, MD, John P. Fischer, MD.
University of Pennsylvania, Philadelphia, PA, USA.
BACKGROUND: Deep sternal wound infection (DSWI) following median sternotomy is associated with considerable complication and morbidity. We aim to develop an actionable risk model of DSWI treated with muscle flaps following median sternotomies at a large single institution.
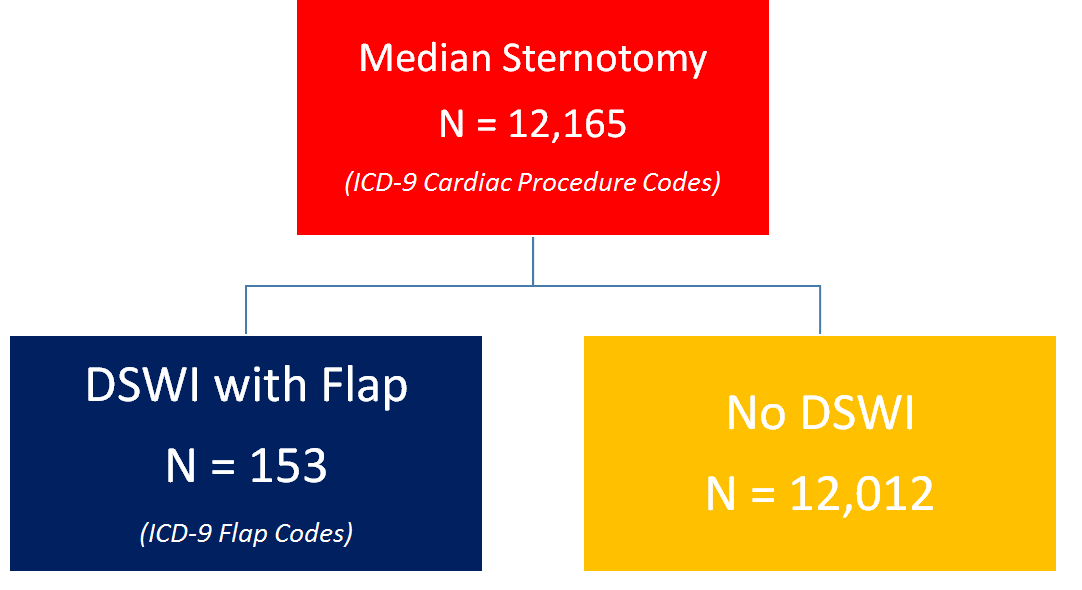
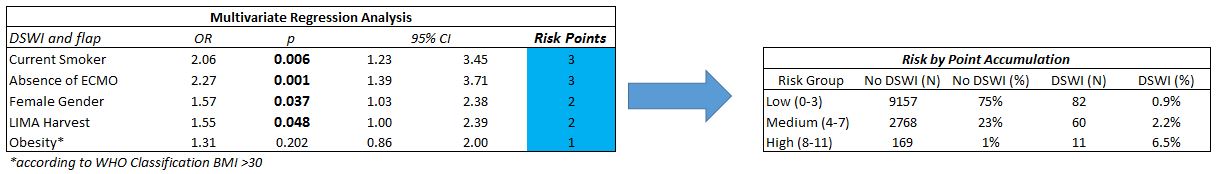
METHODS: All index median sternotomies performed for cardiac procedures from 2008-2014 at our institution were identified via ICD-9 procedure code. Patients were further stratified based on whether or not a flap procedure was performed. Preoperative patient comorbidities and operative characteristics were noted and used to aid in identification of patients at risk for deep sternal wound infection. Logistic multi-variate regression analysis with internal bootstrap validation was performed. Risk factors were weighted and used to create a sternal wound risk assessment tool.
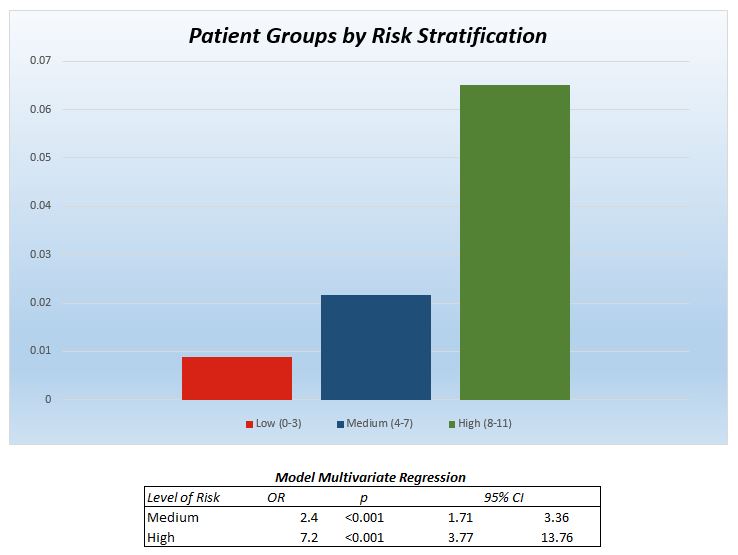
RESULTS: Overall, 12,165 patients underwent median sternotomy with 1.3% (N=153) developing a DSWI treated uniformly with debridement and flap (Figure 1). Index operations included valve procedure (N=7,327), CABG (N=4,633), and lesion excision (N=278). Multivariate regression demonstrated female gender (OR=1.6, p=0.037), LIMA harvest (OR=1.6, p=0.048), absence of ECMO (OR=2.3, p<0.001), and active smoking (OR=2.1, p=0.006) were independently associated with DSWI (Figure 2). Risk factors were weighted to construct a simple decision support tool with a risk distribution as follows: minimal (0.9%), moderate (2.2%), and severe (6.5%) (p<0.001) (Figure 3).
CONCLUSIONS:
We have reviewed a large single center experience with median sternotomy and generated a risk model capable of identifying patients at increased risk for DSWI. This model provides aid in decision support, enables physicians to identify patients that will require more attention post-operatively. This is an accurate and validated risk tool utilizing pre-operative patient data and operative factors to predict DSWI in median sternotomy patients which can be used as an aid in decision support.
Back to 2016 Annual Meeting
|
|
