|
|
|
|
|
Back to 2016 Annual Meeting
Improved outcomes associated with prophylactic plastic surgeon closure of spine surgeries
E. Hope Weissler, Christian Piņa, BA, Michael Ingargiola, MD, Nachi Gupta, MD, PhD, Felipe Molina-Burbano, BS, Peter J. Taub, MD.
Icahn School of Medicine at Mount Sinai, New York, NY, USA.
Introduction: Spine surgeries continue to grow in popularity, recently increasing by more than 200% in a decade. At some institutions, plastic surgeons assist spine surgeons with wound closures of index spine procedures. In anticipation of this becoming a more common practice nationwide, the authors sought to determine whether plastic surgeon closure of spinal wounds as associated with any benefits and to explore risk factors for wound complications in this setting.
Methods: Spine surgeries closed by a single plastic surgeon at a large academic hospital were reviewed. Patients 18 years or younger, with invasiveness indices of zero, current wound infections, or undergoing surgery for management of complications from prior procedures were excluded. Wound complication outcomes were compared with results published in the spine surgery literature using two sample z-tests. Factors significantly associated (p<0.05) with wound complications on univariate analysis were included in a regression model.
Results: Seven hundred eight procedures were done. The average age of the patients was 56±13 years and 38.1% qualified as obese (BMI≥30). Twenty-five patients had any wound complication. Seven patients (1%) had post-operative wound infections and 7 (1%) post-operative wound dehiscence, compared to a study of 22, 430 patients in the ACS-NSQIP database who had an infection incidence of 2.2% (z=2.5, p=0.0116) and 0.3% dehiscence rate (z=3.2, p=0.6336).i Additionally, there were 4 seromas and 7 hematomas. 14 patients (2.0%) required readmission with 30 days. This compares favorably to a meta-analysis of 488,049 patients, in which the pooled 30-day readmission rate was found to be 5.5%ii (z=4.1, p<0.0001). Patients requiring intra-operative blood transfusion (OR 2.68, 1.04-6.93) and with ASA ≥3 (OR 3.77, 1.55-9.14) were more likely to have a wound complication. Surgical time was longer (255.9±134 versus 196±98 minutes, p=0.010) and estimated blood loss higher (1039±956 versus 613.5±788 mL, p=0.006) among patients suffering wound complications. In a multivariate logistic regression controlling for EBL, operative time, ASA status, and intra-operative transfusion, only ASA status of 3 or greater predicted complications (p=0.005).
Conclusions: Plastic surgeon prophylactic closure of spine surgeries was associated with fewer wound infections and readmissions. Contrary to papers in the spine literature that have found operative duration, diabetes, hypertension, and age predictive of complications, we found that only ASA status of ≥3 was associated with wound-related adverse outcomes. This may reflect a lack of power, as the ASA classification includes comorbidities and BMI. Patients at increased risk for complications should be managed more aggressively, including prophylactic local muscle flap closure where appropriate.
Endnotes
i Kimmel KT, Algattas H, Joynt P et al. Risk modeling predicts complication rates for spinal surgery. Spine. 2015;40: 1836-1841. doi: 10.1097/BRS.0000000000001051.
ii Bernatz JT, Anderson PA. Thirty-day readmission rates in spine surgery: systematic review and meta-analysis. Neurosurg Focus. 2015;39(4): 1-9. doi:10.3171/2015.7.FOCUS1534. 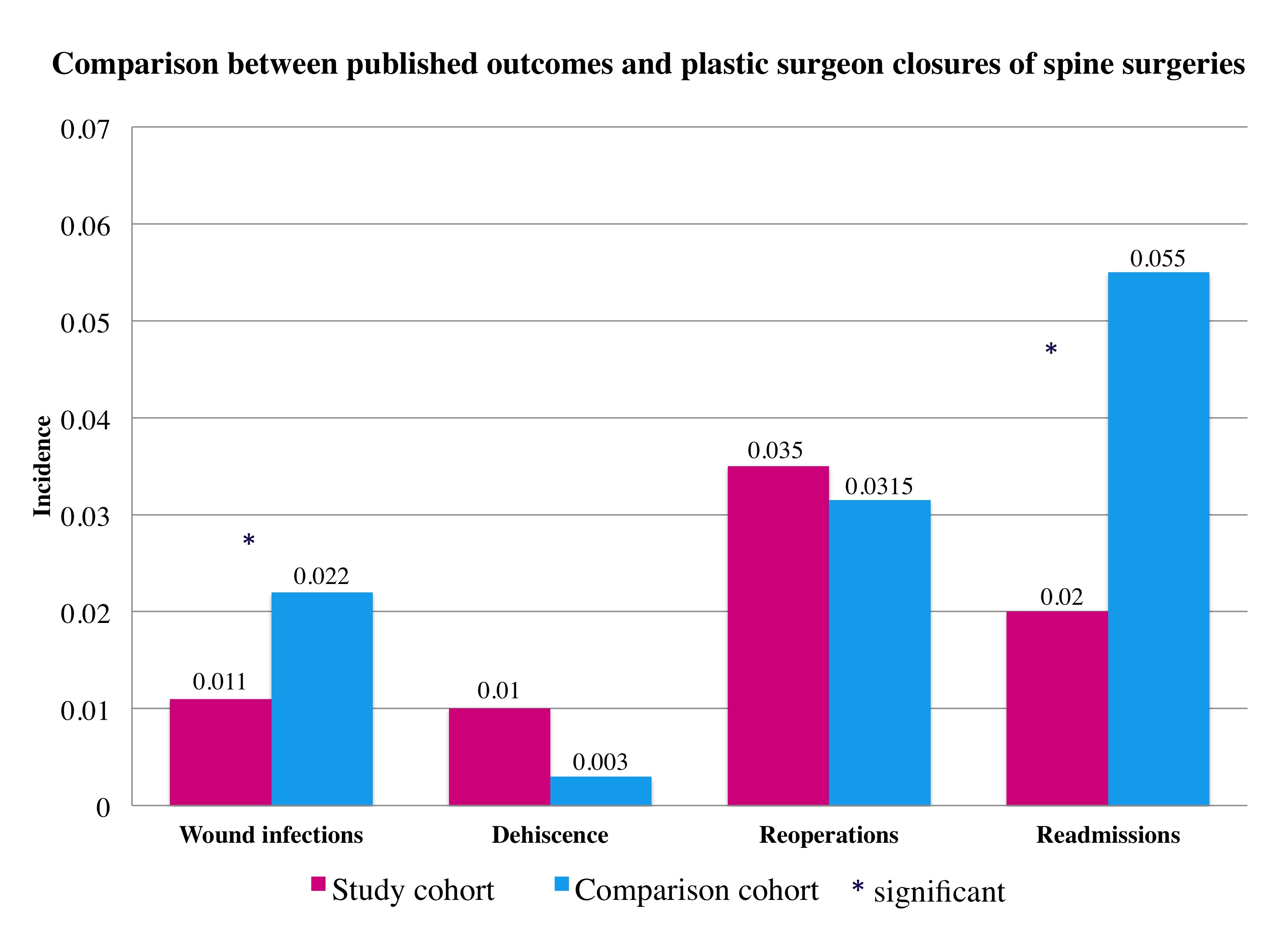
Back to 2016 Annual Meeting
|
|
